Dementia Health Needs Assessment – (Prevention and Care) 2019
This is an assessment of the health needs related to dementia, with a focus on prevention and social care, in Richmond-Upon-Thames, designed with the aim of informing adult social care commissioning activities in the borough.
This document is also available in PDF format: LBRuT Dementia Health Needs Assessment 2019
Executive Summary
Dementia, owing to increasing prevalence and its complex impact on those affected, is now recognised as a major issue nationally and locally. This needs assessment has been constructed to facilitate informed action in response to dementia need in the borough.
How is Richmond affected by dementia?
A higher proportion of Richmond’s population are living with a diagnosis of dementia (0.6%) than average in the rest of London (0.5%). This is, in part, due to the high proportion of people aged ≥65yrs in the borough (15.4%). Approximately 7.2% of this older cohort in Richmond are currently living with dementia. It is anticipated that there will be a 74% increase in the number of people aged ≥65yrs living in Richmond between 2018 and 2035.
In 2018, the cost of dementia in Richmond was approximately £73m, £28.5 of which was attributable to social care costs. This is expected to increase to £126m and £49m respectively by 2035.
How well is Richmond performing in relation to dementia prevention?
Approximately 30% of dementia cases, attributable to the main sub-types of dementia, are potentially preventable. Richmond is performing well in relation to physical inactivity levels and smoking, two of the biggest modifiable risk factors for dementia. However, a high proportion of adults drink more than the recommended ‘safe-limit’ of alcohol per week (35.1%) which increases dementia risk in the population.
Whilst current health promotion activity does address these risk factors, there is no coordinated interagency programme to raise awareness of risk factors specifically in relation to dementia in the borough.
How well is Richmond performing in relation to dementia care?
Following a diagnosis of dementia in Richmond, residents (carers and people diagnosed with dementia) can access support, information and training programmes to equip them with skills to aid in achieving a positive life with dementia. Whilst the pathway to these resources is clear from local memory assessment services, the route from other diagnosing organisations, including hospitals and private care settings, is less well established.
Following the immediate post-diagnostic period, ongoing support is available via clinical, voluntary and social care services. However, navigating what is available and organising care and transport to attend these services can present a challenge for residents.
Typically, progression of dementia leads to greater care needs. With four centres providing day services and two community dementia clinical specialists available for people with dementia, Richmond does have resources to support people in the community as their needs increase. However, residents voice a need for more day centre resources and the caseloads of these clinical specialists are growing.
Once care needs develop beyond the capacity of day centres and home-based care, admission to care homes is often indicated. Whilst care beds in the borough are of a high standard, they are in limited supply; with some residents having to move out of the borough to have their care needs met.
Limitations to this needs assessment
Only one meeting was attended with carers for people with dementia in the borough to hear their perspective on local care. In recognition of this limited community engagement in the needs assessment, any dementia-related work subsequent to this should endeavor to maximise community input.
Furthermore, the data on many metrics for dementia care, particular those related to equity of access, are limited. Consequently, it is not possible to achieve any conclusive insights in to service equity in the borough. Consideration of action to resolve this is included in this document’s recommendations, acknowledging the importance of actively redressing inequity through local authority commissioning and the potential for the burden of dementia to be inequitably distributed based on risk profiles.
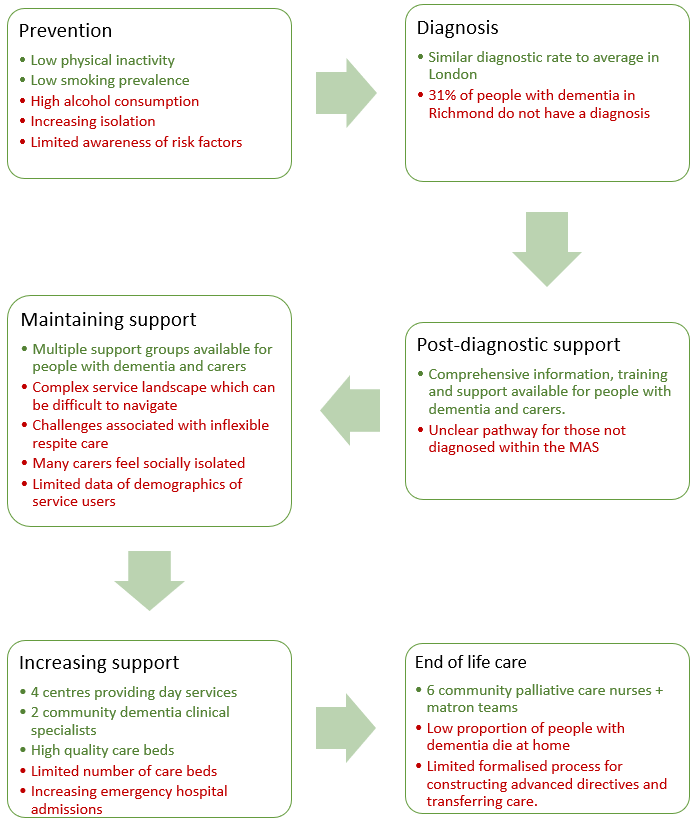
Figure 1: Successes and challenges in dementia prevention and care in Richmond
What dementia is.
Dementia is a group of cognitive and behavioural symptoms associated with a progressive decline in brain functioning. Figure 2 displays some of the brain functions most commonly affected in dementia. Certain sub-types of dementia present with different patterns of functional decline (see Figure 3). Loss of any of these faculties can impact on an individual’s ability to independently live an enjoyable and fulfilling life. However, with the right support and care, people can live well with dementia [i].
Figure 2: Brain functions most commonly affected in dementia.
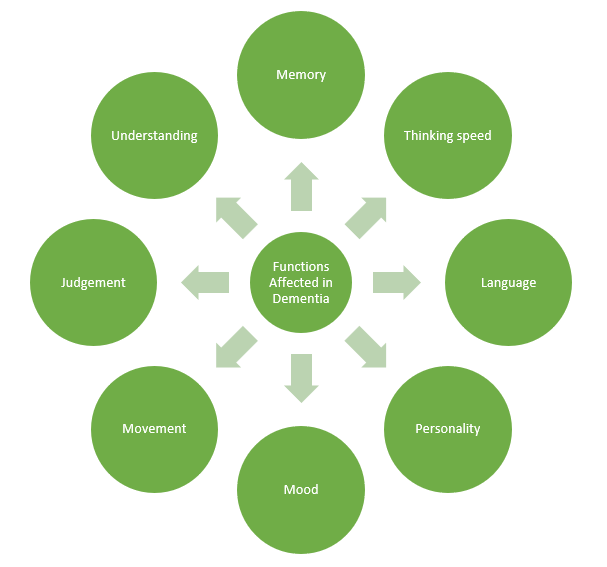
Figure 3: Sub-categories of dementia
| Dementia sub-types |
|
Source: NICE Clinical Knowledge Summaries. May 2017 [iii]
This needs assessment
This is an assessment of the health needs related to dementia, with a focus on prevention and social care, in Richmond-Upon-Thames, designed with the aim of informing adult social care commissioning activities in the borough.
Within this aim, this document has three main objectives:
- To describe population need in relation to dementia, including the needs of those caring for people with dementia in the borough.
- To establish what preventative and social care services are available to meet this need
- To identify gaps in dementia care and preventative service.
- To recommend potential solutions based on best practice and population needs.
Dementia in the UK
Dementia, including Alzheimer’s disease, is now the leading cause of death in England and Wales accounting for 12.7% of all registered deaths (see Figure 4). This is in the context of an anticipated increase in the number of people in the UK living with dementia, from 850,000 in 2018 to approximately 1 million by 2025 [iv].
Figure 4: Graphs describing the trend in proportion of deaths in England and Wales caused by the five leading causes of death in 2017 (2001-2017).
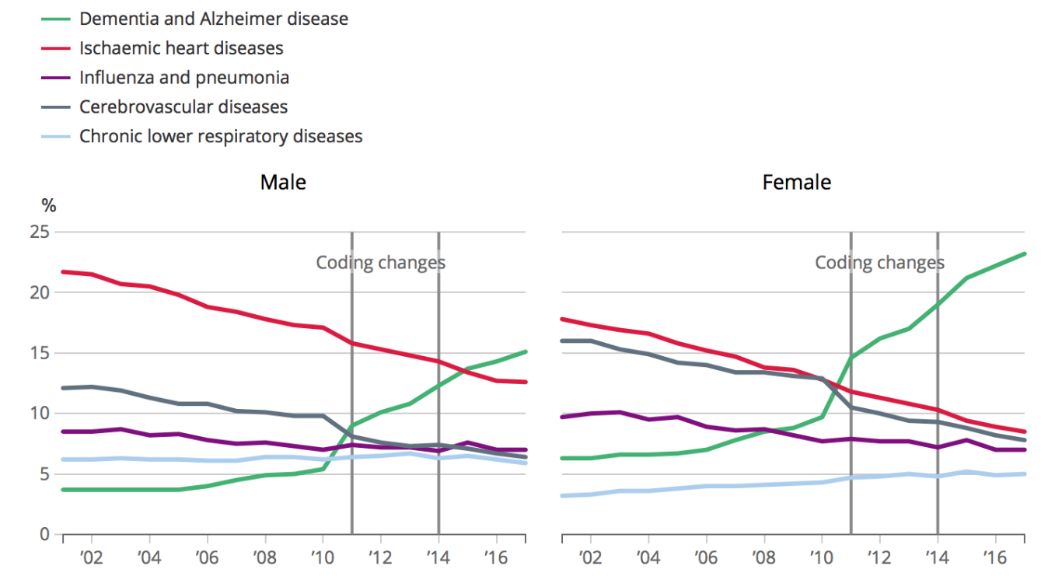
Source: ONS [v]
In acknowledgement of this growing impact, the ‘Prime Minister’s Challenge on Dementia 2020’ (2015) was published. This described the need to improve recognition of dementia, quality of care and strength of community support. The value of ‘dementia friendly communities’ with strong local authority engagement in ‘Dementia Action Alliances’ was also emphasised [vi].
Subsequently, Public Health England (PHE) published a report on Dementia in 2018 highlighting the importance of local authorities’ role in reducing dementia risk through the promotion of healthy lifestyles and maximised use of signposting opportunities[vii]. Additionally, Pharmacy: A Way Forward for Public Health (2017) highlights the potential for local pharmacies to play an impactful role in improving the lives of people with dementia [viii].
The increasing need related to dementia, and disease prevention, nationally is also recognized in the NHS Long Term Plan (2019). The Long Term Plan builds on the Five Year Forward Plan, published in 2014, which declared an ambition to offer “a consistent standard of support for patients newly diagnosed with dementia” [ix], [x].
In addition to appreciating the need for support amongst those with dementia, there is an increasing appreciation of the need to support the growing community of informal carers[1]. Annually, the cost of dementia in the UK is estimated to be approximately £26 billion, £11.6 billion of which is attributable to unpaid care (see Figure 5) [xi]. This indicates the size of the contribution made by informal carers to dementia care. The Carers Action Plan 2018-2020 was published by the DoH. This builds on the 2014 Care Act to further improve recognition of, and support for, informal carers [xii],[xiii].
[1] Informal carers are people who provide care on an unpaid basis.
Figure 5: The cost of dementia in the UK.
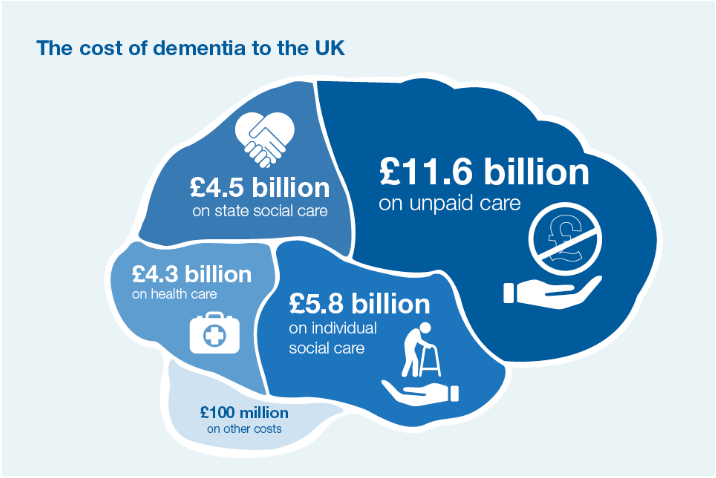
Source: Public Health England[xi].
Dementia in Richmond policy.
This needs assessment builds on themes featured in a variety of documents published in Richmond over the last five years.
The most relevant of which is the Richmond Joint Dementia Strategy. The goals described in this strategy are listed in Table 1. Published in 2016, the Joint Dementia Strategy outlines a plan for dementia care in the borough until 2021. Table 2 highlights other documents published in Richmond relevant to dementia [xiv].
Table 1: Visions of the Richmond Joint Dementia Strategy (2016-2021)
| Visions of the Richmond Joint Dementia Strategy (2016-2021) |
| Maximise prevention opportunities |
| Improve understanding of dementia |
| Prepare the local authority and CCG for the future |
| Provide support for carers as needed |
| Enable people with dementia to live well in Richmond. |
Source: Richmond Joint Dementia Strategy (2016-2021) [xiv]
Table 2: Summary of Richmond policy documents related to dementia.
| Document | Key points related to dementia | Year |
| Joint Mental Health Strategy Implementation Plan for Adults and Older People for Richmond | – Acknowledges that alternative provision in community settings for those with dementia could avoid “a considerable number of unplanned acute admissions”.
– Aims to achieve post-diagnostic support for people with dementia that sustains independence and improves quality of life. – Contains objectives to improve the quality of life for those with dementia through promoting independence, supporting carers and ensuring high quality end of life care. |
2014 |
| Better Care Closer to Home – Richmond Out of Hospital Care Strategy | – Describes the disproportionate impact of dementia on hospital resources
– Acknowledges current pressures on carers. – Aims to improve coordination between hospitals and care homes, improve care home staff training and make Richmond a dementia friendly borough. |
2014 |
| Learning Disability Strategy “Our Big Plan” | – Acknowledges the importance of health promotion for those with learning difficulties.
– Commits to the provision of an appropriate service response to support people with early onset dementia. |
2015 |
| Promoting wellbeing and independence – a framework for prevention | – Acknowledges the capacity for preventative activities to address the rising prevalence of dementia.
– Aims to ensure that each community in the borough works towards becoming a dementia friendly village (community). |
2015 |
| Joint Health and Wellbeing Strategy | – Acknowledges the relationship between loneliness and dementia.
– Refers to the value of dementia friendly villages (communities). |
2016 |
| Housing and Homelessness Strategy | – Recognises the need for affordable extra care accommodation in the borough.
– Describes a need for dementia friendly accommodation. |
2018 |
| End of Life Care Programme (Kingston and Richmond CCGs) | – Described information sharing, co-working, training and carer support in end of life care as areas to improve.
– Does not address dementia end-of-life care specifically. |
2018 |
Overview of dementia in Richmond
New cases of dementia
For those registered with a GP aged ≥65yrs, 9.9 people per 1000 are diagnosed with dementia each year in Richmond [xv]. This is similar to the diagnosis rate, per 1000 people, in London (10.3 per 1000). However, approximately 30.9% of cases of dementia remain undiagnosed in the borough. Therefore, this diagnosis rate is not a true incidence rate [xv].
Implications
As up to 30% of cases of Alzheimer’s disease and vascular dementia are attributable to modifiable risk factors. Richmond’s diagnostic rate highlights the large potential for primary prevention to reduce dementia-related need in the borough[iii].
Current cases of dementia
Amongst those under 65yrs, crude recorded dementia prevalence is 2.47 per 10,000 people (n=50), this is significantly lower than national prevalence (3.41) but similar to regional prevalence (2.28 per 10,000). People aged under 65yrs account for 3.3% of dementia cases in Richmond [xv]. Although comprising a small proportion of cases in Richmond, Young-onset dementia demands particular attention, as services designed for those with older onset dementia are often unsuitable for people with young-onset dementia.
Of those aged ≥65yrs in December 2018, amongst whom dementia is more prevalent, 4.38% of people in Richmond had a diagnosis of dementia (n=1,479) [xv]. This figure climbs to 7.2% of people aged ≥65yrs when those with dementia living without a diagnosis are included in calculations (n=2,201) [xxiii].
In total, in 2017/18, there were 1,497 people with a recorded diagnosis of dementia living in Richmond, equating to 0.6% of the total population. This is a higher proportion than in the rest of London (0.5%).
Based on these figures, and average costs of care per person with dementia as calculated by Alzheimer’s Society, the total cost of care for people with dementia in Richmond is approximately £73 million. Of this, approximately £28.5 million is attributable to social care costs.
Implications
For those already affected by dementia, there remains opportunity to slow disease progression through secondary preventative activities and enhance quality of life with good care provision.
End of Life
The rate of mortality, for people aged ≥65yrs with dementia in Richmond, is 621 per 100,000 people. This is a significantly lower rate than that for London (775 per 100,000) and England (868 per 100,000) [xv]. 237 Richmond residents with dementia died in 2017/18.
16% of those for whom dementia was the underlying cause of death in Richmond in 2016 were born outside of the UK, emphasizing the need to appreciate different cultural requirements during the care and end of life process [xvi].
Implications
At the end of life, people affected by dementia often have an impaired ability to comprehend their environment, in addition to having a reduced capacity for autonomy. Consequently, the palliative care needs of this cohort, required to achieve minimal distress and discomfort, can be significant [xv].
Where are those with dementia living in the borough?
Geographic area
Hampton South has the highest prevalence of diagnosed dementia (1% of those on GP practice lists) of any neighbourhood (MSOA) in Richmond, followed by Twickenham Riverside (0.9%). The neighbourhood with the lowest prevalence of dementia is Twickenham South (0.4%) [xvii]. However, these discrepancies may be partially explained by variations in case finding success rather than true differences in prevalence.
Figure 6, a map of diagnosed dementia prevalence by GP practice in Richmond, gives an indication of how dementia diagnoses are distributed within the borough. Whilst this distribution can act as a proxy to overall prevalence, true prevalence per practice will differ from that displayed, as practice diagnosis rates will vary, with some better at case finding than others. Furthermore, as practice size varies, the actual pattern of variation in the total number of people with a diagnosis of dementia per practice will differ from that shown below. Notwithstanding these limitations, there are two clusters of higher proportions of practice lists having a diagnosis of dementia; southwest Richmond and north/central Richmond.
Figure 6: Prevalence of dementia in Richmond according to GP practice lists, based on QOF data. 2017-18
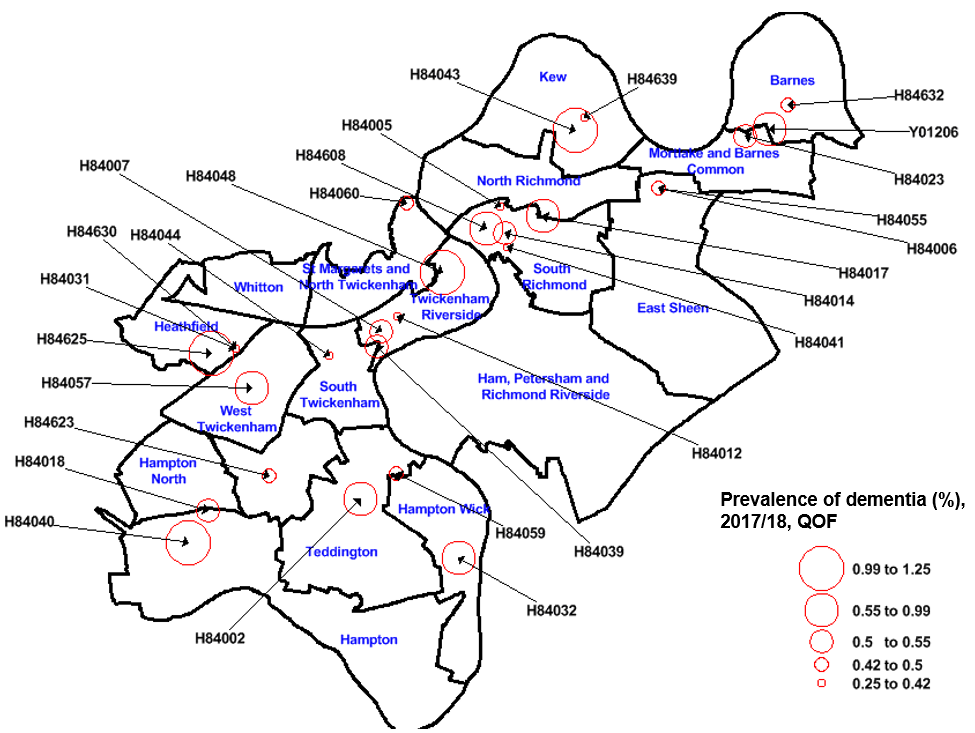
Source: QOF data. See appendix for GP Practice names: Practice code key.
Figure 7 describes the distribution of ASC service users living with dementia in the community in Richmond over the past three years. It appears that a large proportion of those with dementia using ASC services from the community live in southwest and north/central Richmond, consistent with areas of higher prevalence of diagnosed dementia according to GP practice.
Figure 7: Map displaying distribution of adult social care service users living with dementia in the community in Richmond by MSOA between 2015/16-2017/18
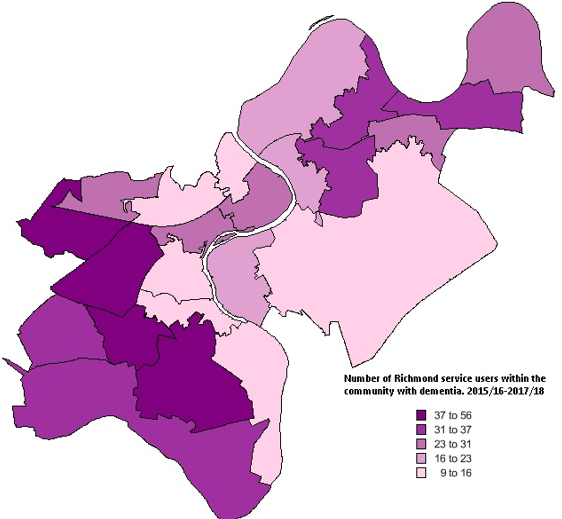
Source: ASC data (Mosaic)
The areas in the borough with the highest proportion of people aged ≥65yrs, i.e. those at higher risk of dementia, are Hampton (19.6%), Hampton North (18.9%), Ham, Petersham & Richmond Riverside (17.3%) and Teddington (17.2%), see Figure 8. This contrasts with St. Margarets & North Twickenham, in which only 9.2% of the population are aged ≥65yrs [xviii].
The size of this intra-borough variation highlights the importance of considering geographic location when allocating resources related to dementia.
In 2016, 129 Richmond residents died, with dementia being considered the underlying cause of death. The four wards with the most residents from this cohort were: Twickenham Riverside (18), Hampton (17), Whitton (15) and Barnes (10). 56% of these 129 people died in a care home (72), 35% died in hospital (46) and 9% died in a private residence (11). The majority of these Richmond residents, who died in hospital, died in West Middlesex Hospital (19) or Kingston Hospital (17)[xix].
Figure 8: Map displaying the proportion of people aged ≥65yrs by ward in Richmond upon Thames differentiated by quantile.
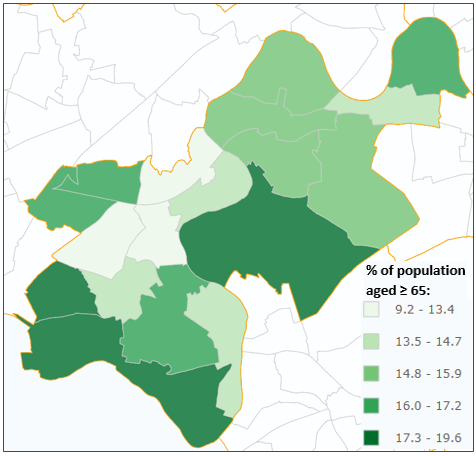
Source: GLA London Ward Profiles (based on 2017 data) [xviii].
Accommodation Type
Based on estimates in the Dementia UK report, published in 2007, approximately 63.5% of people with late-onset dementia live in private households, with 36.5% living in care homes. In Richmond, this would equate to 1,398 people with dementia living in private homes and 803 people with dementia living in care homes [xx].
In 2017/18, of the 550 people receiving services under Richmond Adult Social Care (ASC) living in care homes, 244 (44.4%) had a diagnosis of dementia recorded by the ASC team. When including those not accessing ASC services, those with a diagnosis of dementia not recognised by the ASC team and those living with dementia who do not have a diagnosis, this figure is likely to be much larger [xxi].
Table 3 describes the estimated proportion of people resident in different accommodation settings who live with dementia [xxii]. Applying these proportions, to the numbers of people accessing ASC services, we can estimate that 222 ASC service users living in residential accommodation have dementia, of a total of 383 residents. For nursing homes, the equivalent figure is 122 of 167. Current ASC data counts only 133 people in residential accommodation and 111 people in nursing accommodation having a diagnosis of dementia [xxi].
From this, it may be inferred that 89 people accessing ASC services in Richmond residential homes, and 11 people accessing ASC services in nursing homes, are potentially living with a dementia that is unrecognized by the ASC team, and potentially not recognised at all. This suggests either a greater need for completeness of data collection or for improved access to diagnostic services in residential homes in the borough, or both.
Table 3: Table describing the estimated proportion of people within different care settings with dementia
| Care Setting | Female (%) | Male (%) | Total (%) |
| Extra care housing | 8.8 | 7.9 | 8.1 |
| Residential homes | 62.1 | 52.7 | 57.9 |
| Nursing homes | 75.8 | 67.8 | 73.0 |
| EMI care homes | 90.6 | 86.7 | 90.1 |
Source: Figures extracted from Dementia UK: Second edition (2014) [xxii].
What does the future hold?
The Institute of Public Care (IPC) provide prevalence projections until 2035, shown in Figure 9, which predict a 74% increase in the number of people aged ≥65yrs living with dementia in Richmond between 2018 and 2035 [xxiii].
Figure 9: Predicted number of people with dementia in Richmond divided by sex (2018-2035)
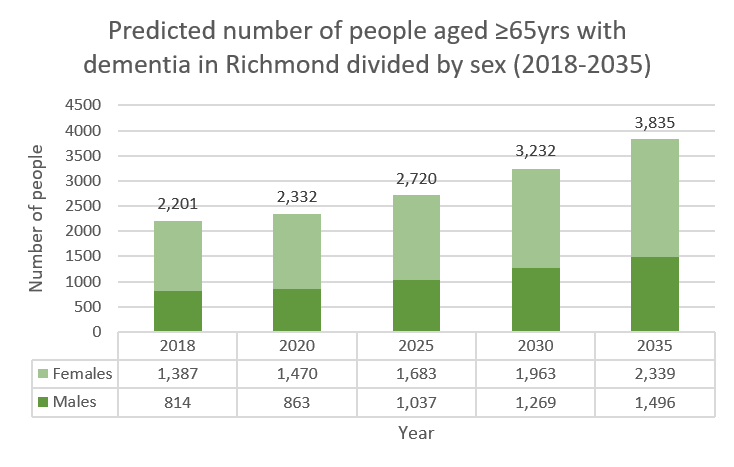
Source: Adapted from IPC data
By 2035, it is anticipated that the number of people aged ≥65yrs living in care/nursing homes will nearly double to 1,549 [xxiii], [xx].
Although these increasing trends are observed, the proportion of people accessing adult social care services who have dementia documented on Mosaic has decreased from 32.8% to 25.9% between
2015/16 and 2017/18. This may be due to reduced quality of data collection rather than a genuine decrease in prevalence.
The proportion of people with dementia receiving ASC services who live in care homes, compared to the proportion living in the community, has increased from 48.9% to 55.1% between 2015/16 and 2017/18 [xxi].
This could suggest that those with early stage dementia living in the community are decreasingly likely to have a diagnosis of dementia, or to have their diagnosis of dementia recognised by the ASC team.
Based on the estimated increase in dementia prevalence suggested in Figure 9, and assuming prevalence of early-onset dementia remains constant, we can estimate that dementia in Richmond in 2035 will cost approximately £125.75 million in 2012/13 prices. The cost of social care alone will be approximately £49million.
What is driving the increasing prevalence of dementia?
The drivers of increasing dementia prevalence can largely[2] be divided into non-modifiable and modifiable risk factors. A modifiable risk factor is a behaviour or environmental exposure which increases disease risk but can be altered; whilst a non-modifiable risk factor is something that increases disease risk and cannot be altered.
[2] Additional factors include phenomena such as migration which are not explored in detail in this report.
Non-modifiable risk factors for dementia
Age is the biggest risk factor for dementia as the impact of stresses on the brain accumulates over time. Beyond the age of 65yrs, risk of dementia approximately doubles every five years (see Figure 10) [xxiv]. Of the 199,419 people currently thought to be living in Richmond, 15.4% are ≥65yrs years old (n=30,631). Between 2018 and 2035, the number of people aged ≥65yrs in Richmond is expected to increase by 73% (see Figure 11). This would mean that 23.4% of the Richmond population will be ≥65yrs in 2035 [xxiii].
Figure 10: Incidence of dementia according to age and sex.
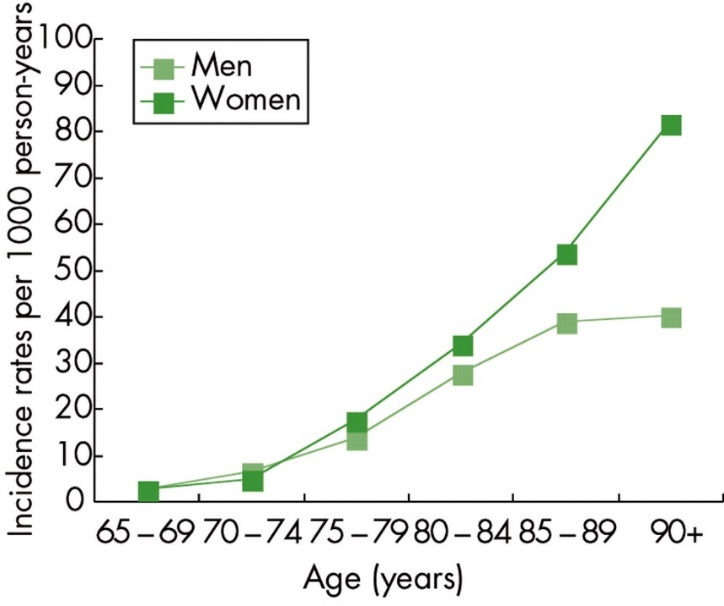
Source: van der Flier WM and Scheltens P. Epidemiology and risk factors of dementia. Journal of Neurology, Neurosurgery & Psychiatry. 2005. 76(5).
Figure 11: Predicted breakdown of age distribution amongst those aged ≥65yrs in Richmond (2018-2035).
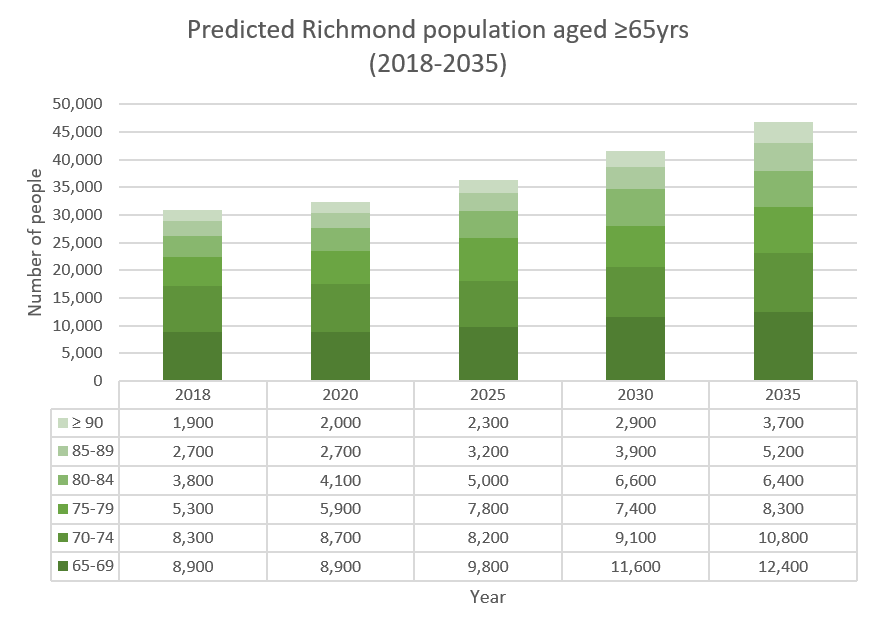
Source: Adapted from IPC data, informed by 2016 ONS data
Other non-modifiable risk factors include genetics, ethnicity and sex.
Most genetic risk factors are not routinely measured in the general population. Consequently, it is difficult to interpret the impact of genetics on risk locally. However, this may change as technology in this field develops. Down’s syndrome, one genetic risk factor for dementia, is recorded more routinely. Prevalence of dementia amongst people with Down syndrome as young as 40-49 is 5.7-55%. This higher prevalence is partially attributable to increased amyloid deposition in the brain[xxv], [xxvi]. There are approximately 80 people with Down’s syndrome aged 18-64 currently living in the borough [xxvii]
Those affected by learning disabilities, other than Down’s syndrome, may also be at higher risk of dementia, although there remains uncertainty about how this risk is conferred [xxviii].According to QOF data, in 2016/17 there were 586 people, known to a Richmond GP, who are affected by a learning disability.
Certain ethnic groups are disproportionately affected by dementia, however the degree to which the environment and genetics are responsible for this difference is unclear. Whilst overall dementia prevalence in the UK is expected to double over the next 40 years, the prevalence of dementia amongst South Asian and Black ethnic groups will increase sevenfold [xliii]. Compared to the 6% of the ≥65yrs population in Richmond who identify as BAME (see Figure 12), 16.3% of Richmond residents that died due to dementia in 2016 were born outside of the UK[3] [xix], [xxiii]. This suggests that the differential risk profiles are manifesting in Richmond.
[3] Ethnicity is not available in PCMD data. If those from the Republic of Ireland are excluded from the cohort born outside the UK this figure falls from 16.3% to 10.1%.
Figure 12: Ethnic groups as a proportion of the total Richmond population aged ≥65yrs
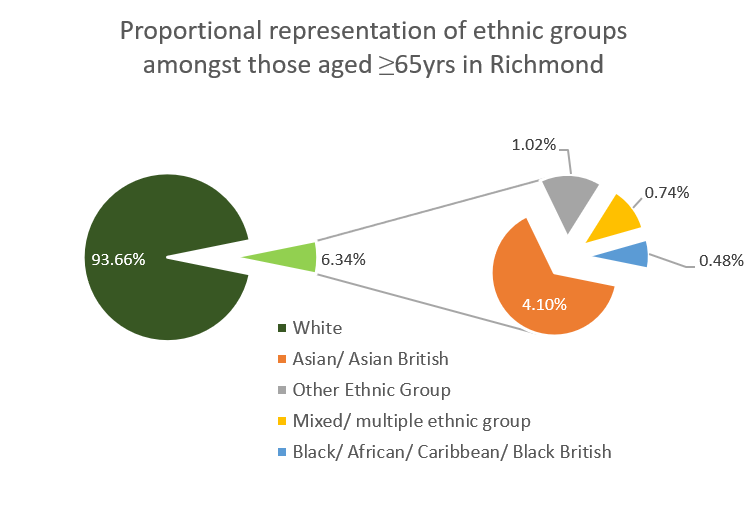
Source: Adapted from IPC site, based on 2011 census data [xxiii].
Women are at higher risk of late-onset dementia whilst men are at higher risk of early-onset dementia (see Figure 9 ). The underlying cause for these differences is uncertain [xxix]. Currently, approximately 63% (n = 1,416) of those aged ≥65yrs in Richmond living with dementia are women. However, women comprise only 56% of the general ≥65yrs population in Richmond (n = 17,000) [xxiii].
Figure 13: Ratio of women to men aged ≥65yrs living in Richmond. compared to ratio of women to men aged ≥65yrs living with dementia in Richmond.
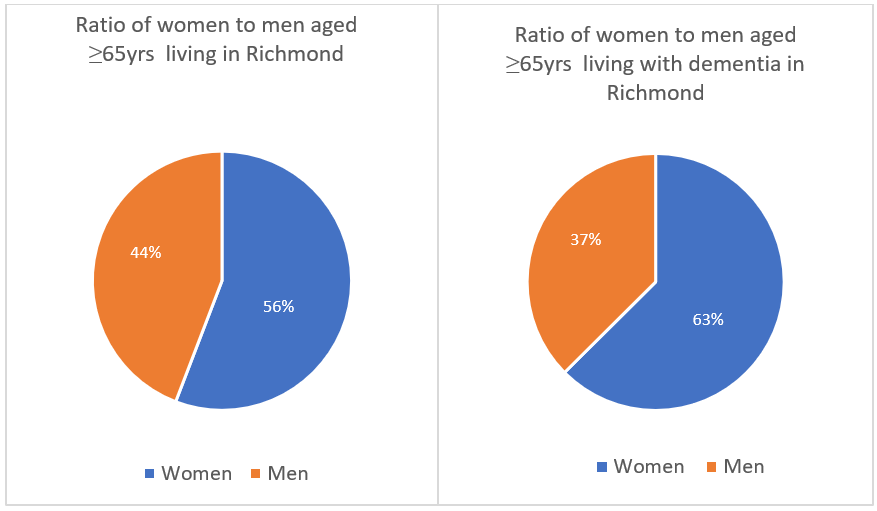
Source: GLA population data and Institute of Public Care data; Source: IPC data.
Modifiable risk factors
As stated above, up to 30% of the most common forms of dementia can be prevented. To achieve such a reduction in the number of people affected by dementia, modifiable risk factors need to be addressed before the onset of disease (see Figure 14). However, even after a diagnosis of dementia, uptake of healthy behaviours can slow disease progression, the potential impact of slowed dementia progression rates by 2050 is shown in Figure 15 [xxx], [xi]. Figure 16 gives an indication of the potential to reduce the cost of dementia care by slowing disease progression [xxx].
Figure 14: Modifiable risk factors for dementia
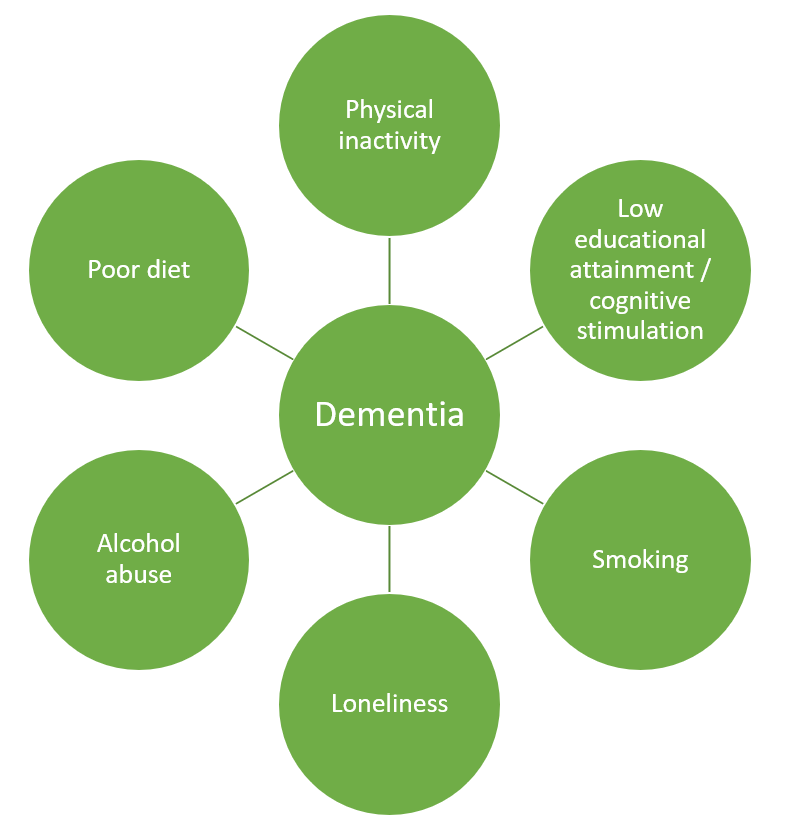
Source: PHE [xi].
Figure 15: Severity of the dementia population in 2050, with slowed progression.
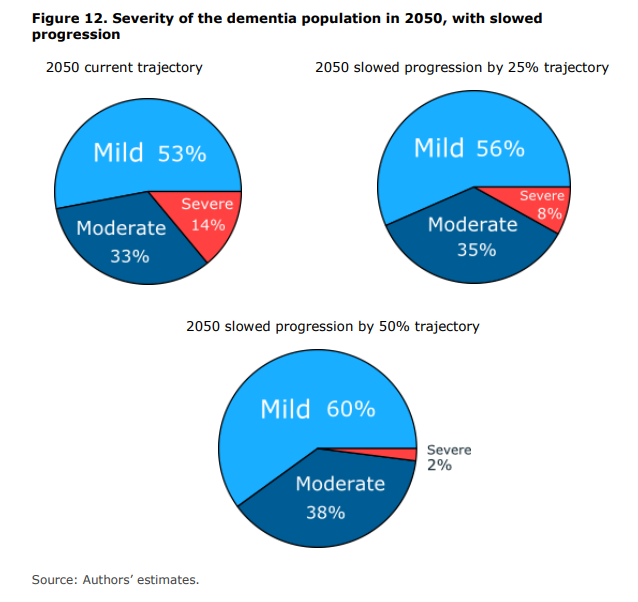
Source: Lewis et al. Office of Health Economics and Alzheimer’s Research UK, 2014 [xxx]
Figure 16: Costs by year and type of cost, with delayed onset of 2 years, mean projections (2011-2050)
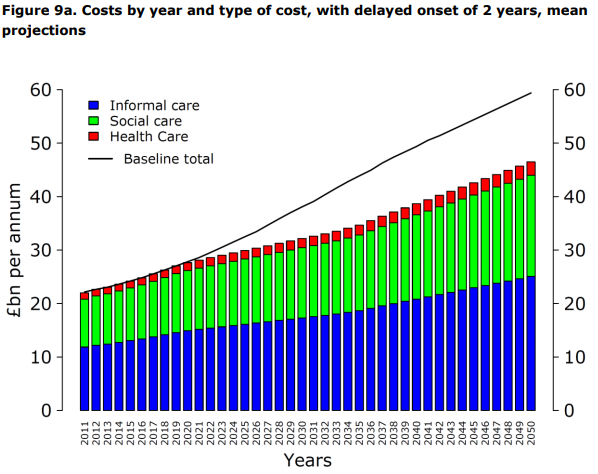
Source: Lewis et al. Office of Health Economics and Alzheimer’s Research UK [xxx]
Physical inactivity
The largest modifiable risk factor for dementia is physical inactivity. Even low intensity exercise, such as walking, can reduce an individual’s risk by around 40% [xxxi]. Although physical inactivity in the borough (17.2%) is significantly lower than average in London (22.2%) and England (22.3%) [xv], physical inactivity does increase risk locally. Based on these figures, modelling suggests that approximately 9.3% (95% CI: 2.4%- 17.6%) of dementia cases in Richmond are attributable to physical inactivity.
Low educational attainment
Low educational attainment follows on from physical inactivity, being attributable for around 7.2% (95% CI: 4.5% – 13.3%) of cases of dementia in the Borough [xxxi]. This impact of early educational activity emphasises the importance of a life course approach in reducing dementia risk.
Smoking
As with many other health conditions, smoking is a major risk factor for dementia, with smokers having between 50-80% higher risk of dementia compared to non-smokers [xxxi], [xxxii]. Currently, adult smoking prevalence in Richmond is 9.8% (n=14,775) [4]. Modelling based on this smoking prevalence suggests that 4.9% (95%CI: 1.3% – 9.3%) of cases of dementia in Richmond are attributable to smoking [xv].
[4] Based on the 2017 Annual Population Survey
Loneliness and isolation
Another modifiable risk factor for dementia is loneliness. Both independently, and through its association with depression, loneliness increases dementia risk. One study suggests that older adults who feel lonely have 1.64 times higher odds of dementia compared to those who don’t feel lonely [xxxi]. It is estimated that only 48.3% of those using adult social care services in the borough feel they have as much social contact as they would like [xv]. The impact of loneliness on dementia in the borough may grow as the number of older people living alone in Richmond increases (see Figure 17) [xxiii].
Figure 17: Graph depicting the predicted number of people aged ≥65yrs living alone in Richmond split by sex (2018-2035)
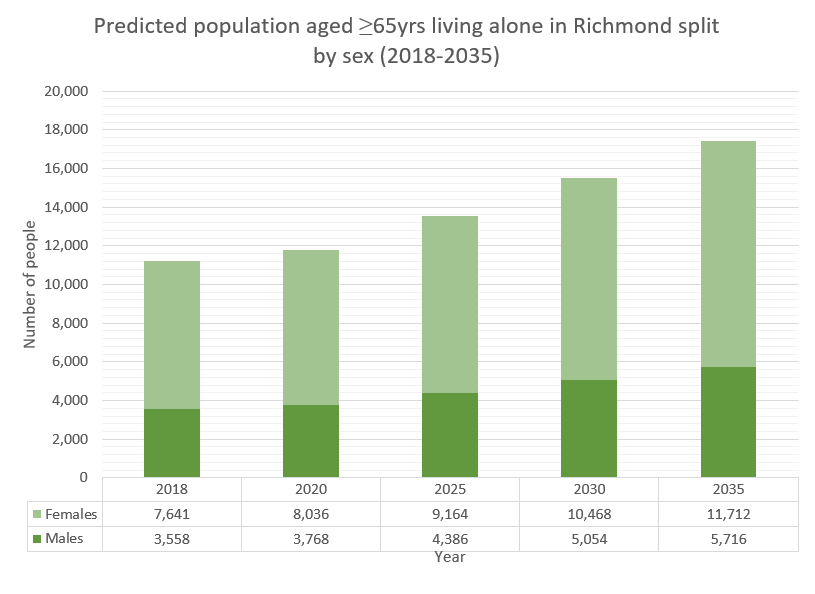
Source: Adapted from IPC data, based on 2016 ONS projections and the General Household Survey of 2007
Alcohol
Alcohol, when consumed regularly in high volumes, can increase dementia risk. Richmond has the third highest proportion of adults drinking to harmful levels (35.1%) in London, but a comparatively low number of people presenting to health services with dependency or acute alcohol-related needs [xv]. Consequently, there appears to be a large cohort of adults in Richmond with hazardous drinking habits who are less likely to be recognized and supported to reduce their risk. This is particularly relevant for young-onset dementia, of which a larger proportion of cases are caused by alcohol use.
Air pollution
Additionally, there is increasing evidence that air pollution may contribute to dementia risk[xxxiii], [xxxiv]. Richmond has been designated as an Air Quality Management Area, due to a high burden of air pollutants, since 2000 [xxxv] .
Diseases associated with dementia
In addition to the modifiable behavioural and environmental risk factors described above, there are also potentially modifiable disease processes related to dementia. Table 4 describes five common diseases associated with an increased risk of dementia. As displayed in the fourth column, many risk factors for these conditions are the same as for dementia, further emphasizing the utility of promoting healthy behaviours in the borough.
Table 4: Description of diseases related to dementia and associated behavioural risk factors.
| Disease | Number of people affected in Richmond | Proportion of dementia cases attributable to disease (95% CI) | Modifiable behavioural risk factors associated with disease and dementia |
| High blood pressure | 23,369 (QOF) | 4.19% (1.2%-8.1%) | Diet, physical inactivity, smoking. |
| Depression[5] | 12,137 (1,410 aged ≥65yrs) | 3.0% (2.0% – 4.2%) | Loneliness, physical inactivity, substance misuse, smoking, low educational attainment. |
| Obesity | 6,741 (QOF) | 1.8% (1.0% – 2.7%) | Diet, physical inactivity. |
| Diabetes | 6,363 (QOF) | 1.2% (0.6%-2.1%) | Diet, physical inactivity. |
| Stroke | N/A | N/A – dementia risk doubled amongst those who have had a stroke | Diet, physical inactivity, substance misuse, smoking. |
Source: PHE and NICE [xv], [xxxi]. [QOF = figure obtained from Quality and Outcomes Framework calculations
The number of people affected by many of these diseases is anticipated to increase in Richmond. By 2035, approximately 10,651 adults will be living with diabetes and 3,992 people aged ≥65yrs will have depression. In addition to increasing dementia risk, co-morbidities increase the risk of hospital admission amongst those living with dementia [xxiii].
Sensory impairment, both hearing and visual, can increase the care needs of people with dementia by reducing an individual’s ability to understand and navigate their environment. The number of older people (≥65yrs) affected by severe hearing loss and moderate or severe visual impairment in Richmond is expected to increase by 74.2% (from 2,384 to 4,153) and 62.8% (from 2,595 to 4,225) respectively between 2017 and 2035 [xxiii].
[5] The risk factors listed for depression are not established as causative.
Understanding the risk factors
A PHE survey in 2015 revealed that, whilst 59% of people know someone with dementia, 21% of the population could not identify any risk factors for dementia. Additionally, only 28% of people recognised smoking and 15% recognised high blood pressure as risk factors for dementia[xxxvi].
What is being done to reduce dementia risks in the borough?
As discussed above, there are many different exposures that can increase dementia risk. Consequently, dementia prevention can be considered as any activity which actively reduces these risks, whether it is explicitly designed with a focus on dementia or not.
Below is an overview of local services related to reducing these risks.
Physical Exercise
Provided via LBRuT:
Richmond council offers a range of sports and fitness activities based in the borough’s 6 leisure centres. Approximately 3500 people are members of these clubs and 200 group exercise classes are attended each week.
The Richmond Inclusive Sport and Exercise (RISE) project is part of the strategic work within the leisure centres focused on supporting those with disabilities access lifestyle services.
Park space, largely maintained by Richmond local authority, is used by private and charity organizations to provide fitness activities, including activities aimed at those aged 50+.
Additionally, there are community-based lifestyle activities delivered by local community groups and facilitated by the council.
Provided via other funding streams:
Additionally, Health walks, a free service supporting group walks for light exercise and social contact, are available locally.
Education and cognitive stimulation
Adult education courses are available at Richmond Adult Community College.
Smoking cessation
The Richmond Stop Smoking Service provides professional support and advice related to multiple aspects of the quitting process. This is funded through LBRuT and is free of charge for residents. This includes access to nicotine replacement therapy.
Isolation and loneliness work
In addition to the social opportunities related to the services above, Age UK Richmond provides a companionship service for older people in the borough. Additionally, there are seven neighbourhood groups who offer different options for befriending and coordinate social events.
Alcohol services
The Richmond Integrated Recovery Service is funded by the local authority, via the public health grant, to treat people with substance misuse issues, including those related to alcohol consumption. At 31st March 2018 there were 626 Richmond residents in treatment with this service, not all of whom were being treated for alcohol dependency.
Recognition and treatment of medical conditions related to dementia
Whilst it is beyond the scope of this needs assessment to comment on the available treatments for all medical conditions related to dementia risk, it is important to note that Richmond continues to provide NHS Health Checks which support recognition of these conditions, in addition to screening for dementia itself. These are free to access for those between 40 and 74 years old.
Following diagnosis, how are those with dementia cared for in Richmond?
Post-diagnostic support
Following a diagnosis of dementia, people in Richmond are often referred to the Alzheimer’s society, who provide support services. ‘Life after diagnosis’ is a 4-week programme with peer involvement intended to facilitate communication and co-support between people recently diagnosed with dementia.
This service is supplemented by the Carers information and Support Programme (CrISP). CrISP 1 is a 4-week course which aims to provided carers with the information about dementia required to most effectively support somebody living with dementia. CrISP 2 is a similar programme aimed at aiding those caring for somebody with dementia after a period of disease progression.
The themes of support in these sessions include information about dementia, advice on important actions in the context of dementia, such as how to establish a lasting power of attorney, and guidance on what other services are available in the borough.
More unstructured support is provided by the borough in the form of caring cafés, dementia support groups and carer support groups. These are environments where people affected by dementia are able to develop social support networks and obtain information relevant to their needs. Multiple attendees at a recent carers meeting in Richmond felt that such social networks are vital for their ongoing wellbeing whilst caring [xxxvii].
Another theme of the same carers meeting was the increasing difficulty in navigating services available for people with dementia, and their carers, in the borough [xxxvii]. Whilst the Alzheimer’s Society provides dementia advisers and support workers who aid navigation, these services are stretched due to scarce resources.
| Funding Mechanism | Organisation | Services provided (days per week) | Number of unique service users |
| Richmond CiLS contract | Age UK | – Dementia support worker (2.5) *
– Dementia friendly activities/signposting (1) |
– One-to-one support: 165
– Activities and peer support: 97 |
| RAID/INS | -Dementia support worker (2.5) *
– Dementia friendly activities/signposting (1) – Two peer support groups for people with dementia |
||
| Voluntary income | Alzheimer’s society | – Community dementia support (6)
– Hospital dementia support (5)
|
– People with dementia and carers: 359 |
| Richmond Carers Contract | Alzheimer’s society | – 2 dementia support workers *
-Support for carers (1) – Carer support groups (4 monthly). |
– One-to-one support: 82
-Peer support: 58 |
| CCG (Young People with Dementia) | Alzheimer’s society | – Dementia support worker *
– Support for people with dementia and carers (0.5) – Peer and carer support groups (0.5) |
-People with dementia and carers: 41 |
| SWLStG | Alzheimer’s society | Dementia Advisor * embedded in Barnes MAS (5) | – People with dementia: 175-200 |
Footnote: * Dementia support workers and dementia advisors provide one to one support, information and advice about living with dementia and caring for someone living with dementia.
Social care after diagnosis
As described above, most people affected by dementia live in private accommodation. Many of those with mild dementia will live independently in this context. However, for people living in private accommodation who are not independent, their care will come from informal sources, formal ‘home care’ provision and day-centre services.
Although not specific to dementia, it is estimated that in 2018, 1,564 people aged ≥65yrs provided ≥ 20 hours of unpaid care per week in Richmond. This figure is predicted to increase to 2,389 by 2035 [xxiii].
This is in comparison to 630 adults living in Richmond receiving formal ‘home care’ when last measured on 31st March 2013. In addition to being less than informal care provision locally, this is less ‘home care’ provision than is provided on average regionally and nationally, proportional to population size.
To supplement this, there are 4 centres which provide day care in the borough (see Table 5). However, the data also describes a deficit in the capacity of these services. In 2013/14, 48.1 per 100,000 (n=220) adults received day care services in Richmond, significantly fewer than average in London and England (268.3 and 301.1 per 100,000 adults respectively) [xv]. During a meeting with local carers for people with dementia, a need for more day centre capacity in the borough was voiced [xxxvii].
Table 5: List of day care centres in Richmond
| Day Care Centres in Richmond | |
| Homelink | A charitable day care centre for people with dementia, and those without dementia, located in Whitton. It caters for those with milder forms of dementia and can host 28 clients per day, between 10am and 3pm, Monday to Friday. Homelink is staffed by nurses and healthcare assistants and provides exercise classes, cognitive stimulation and advice related to benefits. In addition to day care, Homelink host a monthly supper club open to any carers in the area. ‘Carers tea’ is also provided to support carers. |
| Woodville Centre | A day care centre for those with moderate to severe dementia located in Ham. A referral from adult social services is required to attend Woodville centre. The centre has capacity for 35 people to attend from Monday to Friday, with 15 people able to attend on Saturday and Sunday, from 9-5. Activities in the centre include cognitive stimulation and physical exercises. Woodville centre is primarily staffed by health care assistants. |
| Sheen Lane Day Centre | A day care centre primarily for those with physical and/or learning disabilities. This centre has capacity for 25 people to attend from Monday to Friday between 9-5. |
| Elleray Hall | A charitable day-time social centre which provides food and activities for clients, in addition to facilitating access to chiropodists and hairdressers. “Alleviating loneliness in our local community” is the main objective of the centre. |
Note: There are also older person social day centres which can cater for people in the earlier stages of dementia – Barnes Green; Twickenham wellbeing; Whitton centre; The Avenue Centre Kew; Hampton.
Richmond has the lowest proportion of care home beds per 100,000 people aged ≥65yrs in South West London (2,800 per 100,000). There are 46 care homes in Richmond, 29 cater for those aged ≥65yrs, totaling 845 care home beds for those aged ≥65yrs [xxxviii].
PHE calculate that, for every 100 people with a registered diagnosis of dementia in Richmond, there are 41.5 care beds. This is significantly less than the average ratio of beds available in London (51.3 per 100) and England (69.2 per 100) [xv]. During a meeting with palliative care leads in the borough, it was highlighted that, due to a lack of care beds, towards the end of life residents can be displaced out of borough to receive adequate social care [xxxix].
Although few in number, the quality of care beds in Richmond is significantly higher (100% “good or outstanding”) than average in London (51.3%) and England (69.2%) according to the CQC [xv].
Funding for care in Richmond
64% of care home beds in the borough were council funded in 2016/17, a higher proportion than any other borough in South West London, but equal to the average in London. However, this is in the context of relatively few beds existing within the borough. Of the council funded care home placements, 245 were for nursing homes and 300 were for residential homes [xxxii].
Of those using social care in Richmond, 100% (n=612) receive self-directed support, in line with the 2014 care act. This is a significantly higher proportion than average in London (90.2%) and England (88.6%) [xiv].
The medical and social care interface
Emergency admissions
The directly standardized annual rate of emergency admissions to hospital for those aged ≥65yrs with dementia in Richmond in 2016/17 was 3,130 per 100,000[6] (n=973). This is lower than average in London (4,052 per 100,00) and England (3,482 per 100,000) [xv]. However, Figure 18 shows a significant trend of increasing A+E admissions with a mention of dementia in diagnostic coding amongst Richmond residents between 2013/14 and 2017/18 (p = 0.001). Rather than being the primary reason for admission, dementia is more often a secondary or tertiary diagnosis when presenting as an emergency to local hospitals, emphasizing dementia’s relationship to comorbidities [xl] . Whilst the trend in Figure 18 shows a statistically significant positive association between time and emergency admissions, it is not causative. There are many possible underlying causes which may be responsible for this trend, including increasing dementia prevalence, reduced quality/availability of formal dementia care and/or reduced informal care capacity, amongst others.
A higher percentage of those with dementia who are admitted as emergency cases from Richmond have short stays (≤1 night) in hospital (31.7%) compared to average in London (28.9%) and England (28.2%) [xv]. This high proportion of short stays suggests that clinical complexity on presentation may be lower than average regionally and nationally, or that emergency care is more effective locally [xl].
[6] 100,000 members of the general population.
Dementia Sub-type
Interpreting demand for hospital services according to dementia sub-type is challenging as the most common presenting primary diagnosis related to dementia is ‘unspecified dementia’, and coding of late vs. early onset is sparse. However, 68% of those admitted to hospital as an emergency from Richmond with a primary diagnosis related to dementia, other than ‘unspecified dementia’, were admitted with a form of Alzheimer’s disease[7] and 32% with vascular dementia [xl]. This is similar to national dementia sub-type ratios [iii].
[7] This includes ‘mixed Alzheimer’s dementia’.
Figure 18: Number of emergency admissions citing dementia in diagnostic coding amongst Richmond residents between 2013/14 and 2017/18.
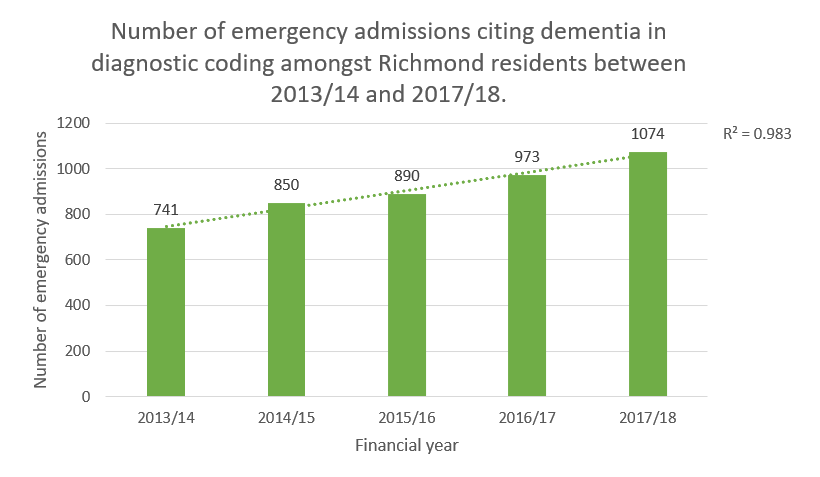
Source: Hospital Episode Statistics. NHS. [p = 0.001; p value relates to two-way significance of positive trend following linear regression]
Discharge
Following admission, the discharge process faces similar challenges as seen nationally. For every 100,000 adults in the borough, 5.6 have transfers of care from hospital to home delayed due to adult social services each year. Unnecessarily prolonged hospital admissions both limit other’s access to hospital services and can increase care needs amongst those being discharged [xv].
Community clinical services
One service designed to avoid admissions to hospital, provided by SWLSTG mental health trust, is the Intensive Community Support Team (previously known as the Intensive Outreach Team). This is a seven-day service which can provide support to carers and daily reviews of people with dementia, for brief
periods, in the community. During normal working hours, this service is supported by a medical doctor who, amongst other activities, can perform medication reviews.
Following discharge from hospital, there is often a brief period of increased need for support whilst people readjust to their home environment. In response to this, 6.8% of those aged ≥65yrs in Richmond receive reablement following hospital discharge (n=201). This is a significantly higher proportion than average regionally and nationally (5.0% and 3.3% respectively) [xv].
This reablement service availability partially explains why more people aged ≥65yrs remain at home 91 days after discharge than average in England (88.1% vs 82.5% respectively). However, since this data was collected in 2013/14, Richmond reablement contracts have changed. Therefore, availability and efficacy may have changed [xv].
As part of the Quality Outcomes Framework (QOF), GPs are incentivised to complete a face-to-face annual review of care plans for people living with dementia. The range of achievement for this QOF metric in the borough is wide, with The Vineyard Surgery and Richmond Green practices achieving 100% and Woodlawn, Hampton Hill, Glebe and North Road Surgeries achieving ≥92% completion. However, Thameside, Richmond Lock, Sheen Lane, Parkshot Medical, Staines road and Essex House practices all achieved ≤ 72% completion. Figure 18 describes the geographical distribution of the high, and low, performing GP practices in the borough.
Figure 19: Map displaying the GP practices with the six highest and six lowest proportions of people with dementia receiving an annual care plan review in 2017-18.
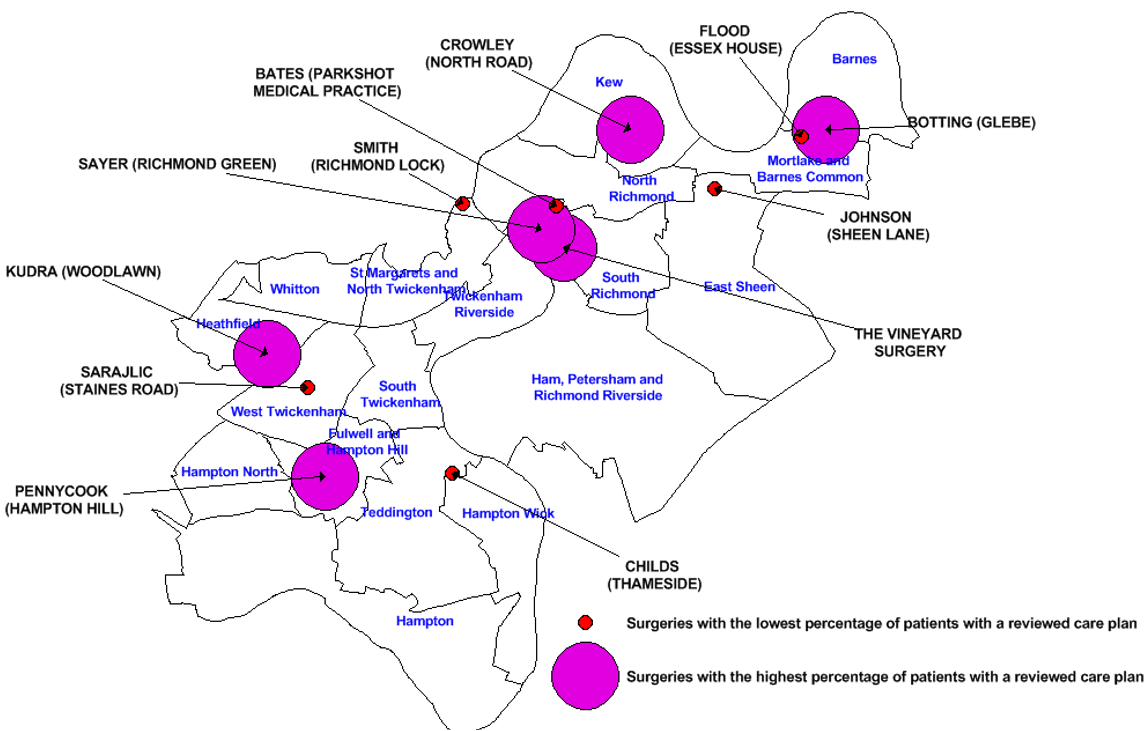
Source: QOF data
End of life care
Dementia is a life-limiting condition and, as stated above, is now the leading cause of death nationally.
Synergy between social and medical care towards the end of life is crucial. In order to achieve adequate comfort in one’s final days, greater support is often required. The extent to which we successfully support residents experience a positive end of life is difficult to measure as each individual will have different needs. In Richmond, in 2016, 53.6% of people with dementia died in their usual place of residence, one metric of palliative care quality. This is a lower proportion than average across England (67.9%), but similar to the proportion in London (55.8%) [xv]. However, an important caveat is that if community care prior to the end of life is very successful and people remain supported at home for longer, instead of living for long periods in nursing homes, they are potentially more likely to need a brief care escalation at the end of life [xxxix].
A tool increasingly used nationwide to improve care, including at the end of life, is ‘coordinate my care’ (CMC). This is an IT resource on which the needs and wishes of people with various medical conditions can be logged. 93% of those who have a CMC record in Richmond have their preferences related to death recorded (i.e. preferred place of death). However, the ratio of people with CMC records to the number of care beds in Richmond is the lowest in south west London [xli].
Palliative care in Richmond is largely provided by Princess Alice Hospice (PAH) and community matron services. There are 6 palliative clinical nurse specialists employed by PAH working in Richmond, these are supported by a small team of carers for emergency situations to provide advice and support symptom control.
Community matron care in the borough is divided into north and south Richmond. There may be some variation in the care provided between these two areas as there is no borough-wide standard for palliative care.
To support end of life care in care homes, the Namaste training course is available via PAH.
Carer support
In 2014/15, carer-reported quality of life scores for people caring for someone with dementia were similar in Richmond to the average in London and England, based on an ASCOF survey. However, carer satisfaction with social services increased between 2012/13 and 2014/15 to become significantly better than average in London (47.1% vs. 35.2% respectively) [xv].
Concerning social isolation of carers, Richmond is performing similarly to the rest of London. However, the fact remains that only 32.1% of adult carers in the borough feel they have as much social contact as they would like, a significantly lower percentage than in 2012/13 (39.0%) [xv].
These figures suggest that the services described above for carers are not comprehensively addressing carers’ social and wellbeing needs in the borough.
Equity of access
As dementia risk is inequitably distributed in society, the need to proactively address equity in access to prevention and care services is paramount. Whilst the following section aims to review how we are promoting equity, current data on Adult Social Care use in relation to demographic features for those living with dementia is limited. Hence, much of the findings described below should be interpreted with caution.
For those with learning disabilities who develop dementia, there is a day centre available specifically aimed at supporting people with learning disabilities in Richmond (Sheen Lane Day Centre) which has capacity for 25 people to attend between Monday and Friday. However, this service is also designed to support people with physical disabilities. Consequently, not all 25 places will be available for those with learning disabilities. In 2017/18, there were 10 people with learning disabilities living with dementia and accessing ASC services in Richmond.
For those with mobility issues, there are two transport services in the borough to facilitate access. However, these are not exclusively available for those affected by dementia. Data on service usage amongst those with dementia is not readily available to determine if this provision is sufficient.
Between 2013/14 and 2017/18, 96.6% of primarily dementia-related admissions were for people of White ethnic origin, consistent with the ethnic profile of the borough [xl]. Of those with a dementia diagnosis in January 2019 in Richmond, 89 identified as White, 39 identified as Asian or Asian British and 16 identified themselves as a member of another ethnic group. This suggests a highly disproportionate representation of people from ethnic minorities amongst those with a diagnosis of dementia in Richmond. However, 90% of people with a diagnosis of dementia in the borough do not have their ethnicity recorded. Consequently, whilst these figures may rationalize further investigation, they should be interpreted with extreme caution[xlii].
Of the 419 people using ASC services in 2017/18, with a diagnosis of dementia recorded by the ASC team and a documented ethnic identity, 91.9% (385) identified as White, 3.1% (13) identified as Asian/Asian British and 2.4% (10) identified as Black/Black British [xxi]. These proportions are similar to the ethnic profile of the total ≥65yrs population in the borough [xxiii].
Although not related to Richmond specifically, there is parity of access to memory clinics between Caucasian and BME communities in London overall [xliii].
Another important domain to consider in relation to dementia is sexual orientation as it is well described that the needs of people identifying as LGBTQI can vary from those identifying as heterosexual[xliv]. In London, in 2017, 89.8% of people identified as heterosexual,2% identified as gay or lesbian, 0.6% identified as bisexual and 0.6% identified as ‘other’ [xlv]. Collection of data on sexual orientation and gender amongst ASC users is not sufficient to understand how needs related to sexual orientation and gender are distributed in the borough.
In relation to sex, similar to national figures, there are over twice as many women with dementia as men amongst those aged ≥65yrs (297 and 126 respectively). However, this relationship is reversed for young-onset dementia [8].
Dementia contributes to health inequity between most and least deprived social groups (see Figure 20). The data to establish if this inequity is addressed through local service provision is not readily available.
[8] Figures too small to be provided in this document.
Figure 20: Graph depicting the breakdown of the life expectancy inequality gap between the most and least deprived deciles for males in England (2014-2016).
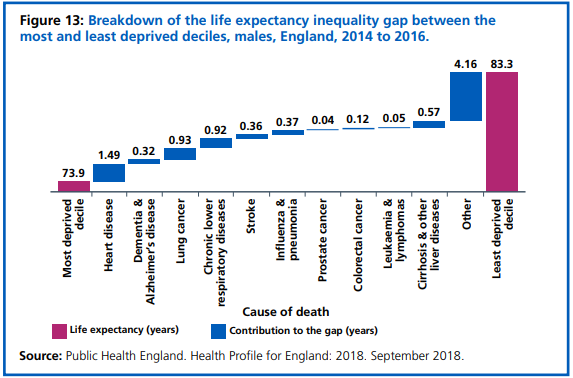
Source: NHS Long Term Plan [ix].
How does dementia prevention and care in Richmond compare to national guidelines?
Prevention
In 2015 NICE guideline 16 was published, ‘Dementia, disability and frailty in later life – mid-life approaches to delay or prevent onset’ (Available from: https://www.nice.org.uk/guidance/ng16 ) [xivi]. The aims of this document are threefold: to reduce modifiable risk factors, to reduce incidence of related non-communicable diseases and to increase resilience through promoting social and emotional wellbeing.
The recommendations within NICE guideline 16, to encourage and facilitate healthy behaviours, are described in Table 6.
Table 6: Table describing NICE guidance 16 recommendations, actions and service gaps relevant to local authority activity.
| Recommendation | Action | Gap(s) |
| Encouraging healthy behaviours | Develop and support population level initiatives | No coordinated inter agency initiatives explicitly related to lowering dementia risk. |
| Integrating dementia risk reduction prevention policies | Incorporate dementia into other health-related policy documents | Limited reference to dementia risk factors in LBRuT policy documents. |
| Raising awareness of risk of dementia, disability and frailty | Commission local campaigns to show how dementia risk can be reduced, even in earlier life | No coordinated local interagency campaigns to increase awareness of dementia and related risk factors. |
| Producing information on reducing the risks of dementia, disability and frailty | Provide advice on risk reduction activities, such as smoking cessation and diet improvement. | Smoking cessation and diet improvement resources available, however limited reference to dementia risk. |
| Preventing tobacco use | Extend smoke-free areas and continue commissioning smoking cessation services. | Smoking cessation services are available. |
| Improving the environment to promote physical activity | Use traffic management and new developments to encourage active travel. | No current activity related to the ‘healthy street’ approach. |
| Reducing alcohol-related risk | Utilise early morning restriction orders and cumulative impact policy as necessary to influence licensing. | There are two cumulative impact zones in the borough and the local public health department review new licensing applications. |
| Supporting people to eat healthily | Limiting the number of unhealthy food outlets and improving access to healthy food. | Food licensing strategy active to limit proximity of unhealthy food outlets to schools. |
Care
For those who have developed dementia, and for carers of people with dementia, NICE guideline 97, published in 2018, was framed around the principles of person-centred care in the context of dementia, [i]. The recommendations most relevant to local authority activity are described in Table 7:
Table 7: Table describing NICE guideline 97 recommendations, actions and service gaps, in relation to local authority activity.
| Recommendation | Action(s) | Gaps |
| Involving people with dementia in decisions about their care | – Provide relevant and accessible information and encourage involvement in decision making.
– Offer early and ongoing opportunities for involvement in advanced decision making. |
– Many carers feel sufficiently involved in decision making in Richmond. However, limited evidence of involvement of people with dementia in decision making.
– Carers describe minimal support with advanced decision making |
| Care coordination | – Provide people living with dementia with a single named health or social care professional who is responsible for coordinating their care who should be involved in developing a care and support plan [9].
– Ensure information can be easily transferred between care settings. – Design services to be accessible as possible |
– Structurally fragmented care provision. Dementia advisors are available but increasingly overstretched and do not provide a complete ‘co-ordination’ role. |
| Interventions to promote cognition, independence and wellbeing | – Offer a range of activities to promote wellbeing which can be tailored to an individual’s needs, including group cognitive stimulation therapy.
– Consider offering cognitive rehabilitation, occupational therapy and group reminiscence therapy. |
– limited availability of regular cognitive stimulation therapy and other evidence-based activities. |
| Assessing and managing other long-term conditions | – Ensure that people living with dementia have equivalent access to diagnosis, treatment and care services for comorbidities to people who do not have dementia. | – Inconsistent primary care provision within care homes.
-Two band 7 health professionals working via HRCH to support people with dementia in a crisis but no dementia specialist nurses available in the borough to support in routine recognition of mismanaged comorbidities. |
| Palliative care | – For people living with dementia who are approaching the end of life, use an anticipatory healthcare planning process involving the person, their carers and their family.
– Support eating and drinking and consider involvement of speech and language therapy. |
– Limited completion of advanced directives
– Comparatively few people with dementia dying at home – Limited utility of tools to coordinate EOL care, such as CMC. |
| Supporting carers | – Offer carers for people living with dementia psychoeducation and skills training intervention.
-Ensure that support provided to carers is personalized and accessible and available after diagnosis and beyond. |
– Limited awareness of/access to psychoeducation resources beyond those provided through Alzheimer Society services following diagnosis.
-Carers perceive that respite care is inflexible and difficult to establish. |
| Moving to different care settings | – “Review the person’s needs and wishes (including any care and support plans and advance care and support plans) after every transition.” | – Minimal evidence of formal consideration of advanced decision making at points of care transfer. |
| Staff training
|
– “Care and support providers should provide all staff with training in person-centred and outcome-focused care for people living with dementia.” | – Lack of clarity regarding proportion of frontline staff that have received appropriate dementia training. Particularly in relation to discussing advanced decisions. |
[9] The Department of Health have produced guidance on how to construct care plans for those with dementia (https://www.england.nhs.uk/wp-content/uploads/2017/11/dementia-good-care-planning-v2.pdf).
Recommendations
Prevention
- LBRuT and Richmond CCG to consider including reference to dementia risk in future local prevention frameworks and any updated strategies related to exercise, education, smoking, alcohol consumption and isolation.
- LBRuT to utilise current local alcohol services, smoking cessation services and exercise/leisure services, where contractually possible, to communicate the beneficial impact of making positive lifestyle changes on dementia risk.
- LBRuT to work with SWL STP and Richmond CCG to create a consistent and coordinated multi-agency communication strategy to improve awareness of dementia risk in the borough. This may be based on the national campaign ‘what’s good for your heart is good for your brain’ [xlvii].
- Use resources available within Making Every Contact Count work to increase frontline workforce awareness of dementia and the potential for prevention.
- Recognising increased risk of dementia within the BAME community, LBRuT should consider improving data collection on service use to ensure needs are being met equitably. Additionally, proactive methods to increase awareness of the value of preventative activities in these communities should be considered.
- Appreciating the positive impact of exercise on dementia risk, LBRuT should review how we can transform physical infrastructure in the borough to promote active travel, potentially in accordance with the ‘Healthy Streets’ initiative [xlviii].
- LBRuT should consider formally reviewing activities provided, by day services, day centres and care homes in the borough for those with dementia, to recognize and/or support adherence to national evidence-based guidance and/or support, e.g. cognitive stimulation therapy and group reminiscence therapy.
Care
Coordination of care
- In response to the challenges some residents face in navigating local services, LBRuT and the CCG could consider, in collaboration, the potential to establish a named and accountable care coordinator, such as that described in a recent NICE report [xlix].
- An additional activity the council can consider, in relation to service navigability, is to create a single point of access to information about local dementia services.
- Acknowledging the lack of standardised access to post-diagnostic services following diagnosis outside of the memory assessment services, Richmond CCG, SWL STP and SWLSTG MHT could consider reviewing current referral pathways.
- Building on previous Dementia Action Alliance work in the borough to build engagement of multiple stakeholders in dementia care, LBRuT could work to re-establish regularity in DAA meetings [l].
- To support in the coordination of end of life care, LBRuT, Richmond CCG, SWLSTG and PAH should consider collaboratively creating a standardised document, capturing needs, wishes and advanced decisions of those affected by dementia to use when care is transferred between organisations.
- Due to inconsistencies in access to primary care for those with dementia living in local care homes, LBRuT and Richmond CCG should consider reviewing the potential for standardizing primary care accessibility for this cohort. Additionally, efforts should be made to standardise the quality of primary care provided to those living in private accommodation, e.g. increasing the number of practices providing an annual face to face care plan review for all people with dementia.
Quality of care and support.
- LBRuT and Richmond CCG could collaboratively work to ensure recognition of dementia in local care homes is optimized and recorded effectively when recognised.
- Continue to develop Richmond’s communities into dementia friendly communities to reduce isolation and improve community engagement possibilities for those affected by dementia [li].
- In response to incomplete data on the ethnicity and sexual orientation adult social service recipients, and the limits this places on measuring equity of service distribution, LBRuT could consider auditing current data collection methods. The learning from this process could be shared amongst other agencies.
- Additionally, in recognition of the disproportionate impact of dementia in Richmond, proactive measures to increase awareness of, and access to, care services amongst BAME and economically deprived communities should be considered whilst awaiting data to permit a more focused approach.
- Recognising the anticipated increase in sensory impairments in Richmond, and the potential for these to exacerbate dementia, LBRuT and Richmond CCG could consider reviewing the need to standardize access to screening services, where appropriate, within local day centres and care homes
- Due to limited information on current dementia training in the borough; LBRuT, Richmond CCG and South West London and St George’s Mental Health Trust could consider an audit of the proportion of frontline care professionals who have completed NICE recognized dementia awareness training.
- Consider increasing availability and flexibility of respite care, including day care centres, and home care to facilitate carer wellbeing and reduce isolation (see the 2004 NHS Service Delivery Organisation document)[lii], [liii], [liv], [lv].
- To prepare for an increase in dementia prevalence, in the context of limited care beds in the Borough, LBRuT could review capacity to increase the number of care beds available locally.
- Consider the geographical distribution of dementia need described within this report. when commissioning services, including potential obstacles to accessing different sites (e.g. transport links).
- Recognising the lack of engagement of those directly affected by dementia in this document, people with dementia and carers for people with dementia should be actively involved in any future actions.
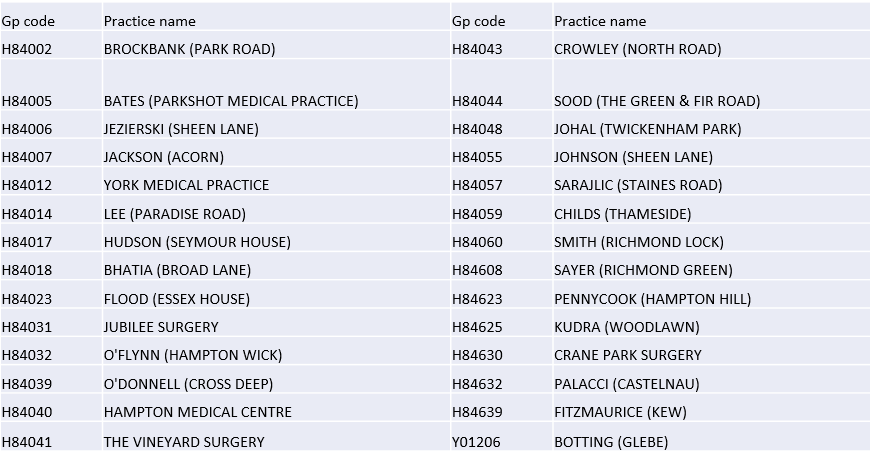
Appendix
Richmond GP practice name: practice code key
References
[i] National Institute for Health and Care Excellence. Dementia: assessment, management and support for people living with dementia and their carers. NG97. June 2018. Available from: https://www.nice.org.uk/guidance/ng97
[ii] National Health Service. Dementia Guide. June 2017. Available from: https://www.nhs.uk/conditions/dementia/about/
[iii] National Institute for Health and Care Excellence. Clinical Knowledge Summaries. Dementia. May 2017 [Cited 15 Oct 2018]. Available from: https://cks.nice.org.uk/dementia
[iv] Office for National Statistics. Deaths registered in England and Wales (series DR): 2017. [Cited on 13 Nov 2018]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsregisteredinenglandandwalesseriesdr/2017
[v] ONS, Deaths registered in England and Wales (series DR) 2017. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsregisteredinenglandandwalesseriesdr/2017
[vi] Department of Health. Prime Minister’s challenge on dementia 2020. 2015 [Cited 16 Oct 2018]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/414344/pm-dementia2020.pdf
[vii] Public Health England. Dementia: applying All Our Health. Jan 2018 [Cited 16 Oct 2018]. Available from: https://www.gov.uk/government/publications/dementia-applying-all-our-health/dementia-applying-all-our-health
[viii] Public Health England. Pharmacy: A Way Forward for Public Health, Opportunities for action through pharmacy for public health. September 2017. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/643520/Pharmacy_a_way_forward_for_public_health.pdf
[ix] National Health Service. NHS Long Term Plan. January 2019. Available from: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan.pdf
[x] National Health Service. Five Year Forward View. October 2014. [Cited 09 Nov 2018]. Available from: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
[xi] Public Health England. Health matters: midlife approaches to reduce dementia risk. Mar 2016 [Cited 16 Oct 2018]. Available from: https://www.gov.uk/government/publications/health-matters-midlife-approaches-to-reduce-dementia-risk/health-matters-midlife-approaches-to-reduce-dementia-risk
[xii] Department of Health & Social Care. Care Act. 2014. (http://www.legislation.gov.uk/ukpga/2014/23/contents/enacted)
[xiii] Department of Health and Social Care. Carers Action Plan 2018-2020. [Cited 14 Nov 2018]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/713781/carers-action-plan-2018-2020.pdf
[xiv] London Borough of Richmond upon Thames. Joint Dementia Strategy, 2016-2021. 2016. [Accessed online 21 Nov 2018] Available from: https://www.richmond.gov.uk/media/13380/joint_dementia_strategy_2016_21.pdf
[xv] Public Health England. Public Health Profiles. Available from: https://fingertips.phe.org.uk/
[xvi] Primary Care Mortality Database. 2016
[xvii] House of Commons Library. Constituency data: how healthy is your area? January 2019. Available from: https://commonslibrary.parliament.uk/social-policy/health/diseases/constituency-data-how-healthy-is-your-area/
[xviii] Greater London Authority. Ward Profiles and Atlas. Available from: https://data.london.gov.uk/dataset/ward-profiles-and-atlas
[xix] NHS Digital. Primary Care Mortality Database. 2016
[xx] Knapp M, Prince M et al. Dementia UK, the full report. 2007. [Cited 15 Nov 2018]. Available from: http://www.the-debenham-project.org.uk/downloads/articles/dementiauk.pdf
[xxi] Richmond Local Authority. Mosaic adult social care database. 2019.
[xxii] Alzheimer’s Society. Dementia UK, second edition. 2014. Available from: http://eprints.lse.ac.uk/59437/1/Dementia_UK_Second_edition_-_Overview.pdf
[xxiii] Institute of Public Care. Projecting Older People Population Information. [Cited 11 Nov 2018] Available from: http://www.poppi.org.uk/index.php
[xxiv] van der Flier WM and Scheltens P. Epidemiology and risk factors of dementia. Journal of Neurology, Neurosurgery & Psychiatry. 2005. 76(5). Available from: https://jnnp.bmj.com/content/76/suppl_5/v2
[xxv] Prasher VP and Mahmood H. Management of Dementia in Intellectual Disability. Chapter 11: 136-137. Seminars in the Psychiatry of Intellectual Disability. 2019 Cambridge University Press
[xxvi] Head E, Powell D, Gold BT and Schmitt FA. Alzheimer’s Disease in Down Syndrome. Eur J Neurodegener Dis. 2012; 1(3): 353-364. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4184282/
[xxvii] Institute of Public Care, Projecting Adult Needs and Service Information. [Cited 11 Nov 2018]. Available from: http://www.pansi.org.uk/
[xxviii] Strydom A, Hassiotis A, King M and Livingston G. The relationship of dementia prevalence in older adults with intellectual disability (ID) to age and severity of ID. Pyschological Medicine. Jan 2009 39(1): 13-21.
[xxix] Podcasy JL and Epperson CN. Considering sex and gender in Alzheimer disease and other dementias. Dialogues in Clinical Neuroscience. 2016 18(4):437-446. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5286729/
[xxx] Lewis F, Schaffer SK, Sussex J, O’Neill P and Cockcroft L. Alzheimer’s Research UK and Office of Health Economics. The Trajectory of Dementia in the UK – Making a Difference. 09 Jun 2014. Available from: https://www.alzheimersresearchuk.org/wp-content/uploads/2015/01/OHE-report-Full.pdf
[xxxi] National Institute of Health and Care Excellence. Clinical Knowledge Summaries. Dementia Risk factors. May 2017 [Cited 19 Nov 2018]. Available from: https://cks.nice.org.uk/dementia#!backgroundsub:2
[xxxii] Cataldo JK, Prochaska JJ and Glantz SA. Cigarette smoking is a risk factor for Alzheimer’s disease: An analysis controlling for tobacco industry affiliation. J Alzheimers Dis. 2010; 19 (2): 465-480. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2906761/
[xxxiii] Chen, H., Kwong, JC., Copes, R., Hystad, P., van Donkelaar, A., Tu, K., Brook, JR., Goldberg, MS., Martin, RV., Murray BJ., Wilton, AS., Kopp, A. and Burnett, RT. Exposure to ambient air pollution and the incidence of dementia: A population-based cohort study. Environ Int. 2017 Nov; 108:271-277. [Accessed online] Available from: https://www.ncbi.nlm.nih.gov/pubmed/28917207
[xxxiv] Carey, IM., Anderson, HR., Atkinson, RW., Beevers, SD., Cook, DG., Strachan, DP., Dajnak, D., Gulliver, J. and Kelly, FJ. Are noise and air pollution related to the incidence of dementia? A cohort study in London, England. BMJ Open. 2018 Sep 11;8(9). [Accessed online] Available from: https://www.ncbi.nlm.nih.gov/pubmed/30206085
[xxxv] Department for Environment Food & Rural Affairs. UK Air. Local Authority Details, London Borough of Richmond. Available from: https://uk-air.defra.gov.uk/aqma/local-authorities?la_id=352
[xxxvi] Public Health England. British Social Attitudes: Attitudes to dementia. 2015. Available from: https://www.natcen.ac.uk/media/1264339/d%C2%A3mntla.pdf
[xxxvii] Meeting with carers for people with dementia. Woodville day centre. 11 Jan 2019.
[xxxviii] South West London STP. Care Home Data Pack. September 2018.
[xxxix] Meeting with palliative care community leads. Princess Alice Hospice Education Centre 14/01/2019.
[xl] NHS England. Hospital Episode Statistics. 2018.
[xli] South West London STP. Care Home Data Pack. September 2018.
[xlii] NHS Digital. Recorded Dementia Diagnoses – January 2019. 12 Feb 2019. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/recorded-dementia-diagnoses/january-2019
[xliii] Cook, L., Mukherjee, S., McLachlan T., Shah R., Livingston, G., Mukadam, N. Parity of access to memory services in London for the BAME population: a cross-sectional study. Aging & Mental Health. 12 Mar 2018 [Cited 16 Oct 2018]. [Accessed online] Available from: https://www.tandfonline.com/doi/abs/10.1080/13607863.2018.1442413?journalCode=camh20
[xliv] Alzheimer’s Society. LGBT: Living with dementia. [Online; Accessed Mar 2019] Available from: https://www.alzheimers.org.uk/get-support/daily-living/lgbt-living-dementia
[xlv] Office for National Statistics. Sexual Identity, subnational. 19 April 2017. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/sexuality/datasets/sexualidentitysubnational
[xivi] National Institute for Health and Care Excellence. Dementia, disability and frailty in later life – mid-life approaches to delay or prevent onset. NG 16. 2015. Available from: https://www.nice.org.uk/guidance/ng16
[xlvii] Department of Health. Living well with dementia: A National Dementia Strategy. Feb 2009. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/168220/dh_094051.pdf
[xlviii] Transport for London. Healthy Streets. [Online, Accessed Feb 2019]. Available from: https://tfl.gov.uk/corporate/about-tfl/how-we-work/planning-for-the-future/healthy-streets
[xlix] National Institute of Health and Care Excellence. Tailored resource: The named care coordinator role from the perspective of older people. 15 July 2016. Available from: https://www.nice.org.uk/guidance/ng22/resources/practice-examples-the-named-care-coordinator-role-in-practice-pdf-3308714149381
[l] Dementia Action Alliance. 2019. Available from: https://www.dementiaaction.org.uk/
[li] Alzheimer’s Society. Dementia-friendly communities. Available from: https://www.alzheimers.org.uk/get-involved/dementia-friendly-communities
[lii] Arksey H, Jackson K, Croucher K, et al. 2004. Review of respite services and short-term breaks for carers of people with dementia. Available from: http://eprints.whiterose.ac.uk/73255/
[liii] Roberts E and Struckmeyer KM. The Impact of Respite Programming on Caregiver Resilience in Dementia Care: A Qualitative Examination of Family Caregiver Perspectives. Inquiry. 2018 Vol 55. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5808833/
[liv] Tretteteig S, Vatne S and Rokstad AM. The influence of day care centres designed for people with dementia on family caregivers – a qualitative study. BMC Geriatrics. 2017; 17 (1): 5. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5216603/
[lv] Vandepitte S, Van Den Noortgate N, Putman K, Verhaeghe S, Verdonck C and Annemans L. Effectiveness of respite care in supporting informal caregivers of persons with dementia: a systematic review. Geriatric Psychiatry. June 2016: 31(12): 1277-1288. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/gps.4504
Document Information
Acknowledgements
| Dr Samuel Rigby | Public Health Registrar | London Borough of Richmond upon Thames, Public Health Department |
| Hana Alipour-Mehraban | Senior Commissioning Manager | London Borough of Richmond upon Thames, Adult Social Services |
| Shannon Katiyo | Public Health Consultant | London Borough of Richmond upon Thames, Public Health Department |
| Sally Bahri | Intelligence Analyst | London Borough of Richmond upon Thames, Business Intelligence Team |
| Jennifer Nsubuga | Mental Health Transformation Project Manager | SWL Health and Care Partnership |
| Dr Stavroula Lees | Mental Health Lead | Richmond CCG |
List of abbreviations:
APOE-4: Apolipoprotein E4 (a gene related to increased dementia risk).
AS: Alzheimer’s Society
CCG: Clinical Commissioning Group
CiLS: Community Independent Living Service
CMC: Co-ordinate My Care
CrISP: Carers Information and Support Programme
CQC: Care Quality Commission
DLB: Dementia with Lewy bodies
EOL: End of Life
FTD: Frontotemporal dementia
GLA: Greater London Authority
HES: Hospital Episode Statistics
INS: Integrated Neurological Services
IPC: Institute of Public Care
LA: Local Authority
LBRuT: London Borough of Richmond upon Thames
LGBTQI: Lesbian, gay, bisexual, transgender, questioning and intersex
LSE: London School of Economics
Mosaic: Adult Social Care service user database
NHS: National Health Service
NICE: National Institute for Health and Care Excellence
ONS: Office for National Statistics
PAH: Princess Alice Hospice
PHE: Public Health England
QOF: Quality and Outcomes Framework
RAID: Richmond Aid
SWLStG: South West London and St Georges (mental health trust)
UK: United Kingdom
