Richmond upon Thames Suicide and Self-Harm Prevention Strategy 2019-2022
Richmond upon Thames Council, Richmond CCG 2020
The strategy is also available in PDF format: LBRuT Suicide and Self-Harm Prevention Strategy 2019-2022
Executive Summary
Vision
Our vision is that Richmond will be a home to communities that are described as happy, thriving and resilient.
We believe that with the right support at the right time, people can recover from psychological distress and mental disorder.
We believe suicide is preventable and aim to ensure individuals;
- value their own life and the lives of others
- should never feel that suicide is the only option
- are supported in times of need, by safe, integrated, and compassionate services
Aim
The overall aim of this strategy is to reduce the rate of suicide, suicidal behaviour and self-harm through the following objectives:
Objectives
This strategy aims to:
- Improve understanding of local need – Suicide audit, pathway mapping and needs assessment
- Challenge the stigma and discrimination associated with mental disorder by:
- Increasing awareness of mental health and mental disorder
- Adopt more sensitive media reporting in relation to mental disorder, self-harm and suicide
- Improve access to information and Postvention Support – for those concerned or affected by suicide
- Prevent self-harm amongst young people – Support the development of the CAMHS Local Transformation Plan including prevention in schools, effective care pathways and A&E liaison services
- Improve access to services – Increase the numbers of people from high risk groups accessing appropriate services
- Improve crisis responses and pathways – Improvements in crisis care pathways and closer integration of mental health and substance misuse services, safer discharge, improved crisis planning.
Governance
This Strategy has been agreed by the Crisis Care Concordat and approved by the Health and Wellbeing Board. The Crisis Care Concordat will be responsible for overseeing the progress and delivery of the action plan and will report back to the Health and Well-being Board on an annual basis.
1. Where are we now?
1.1 Richmond upon Thames Profile
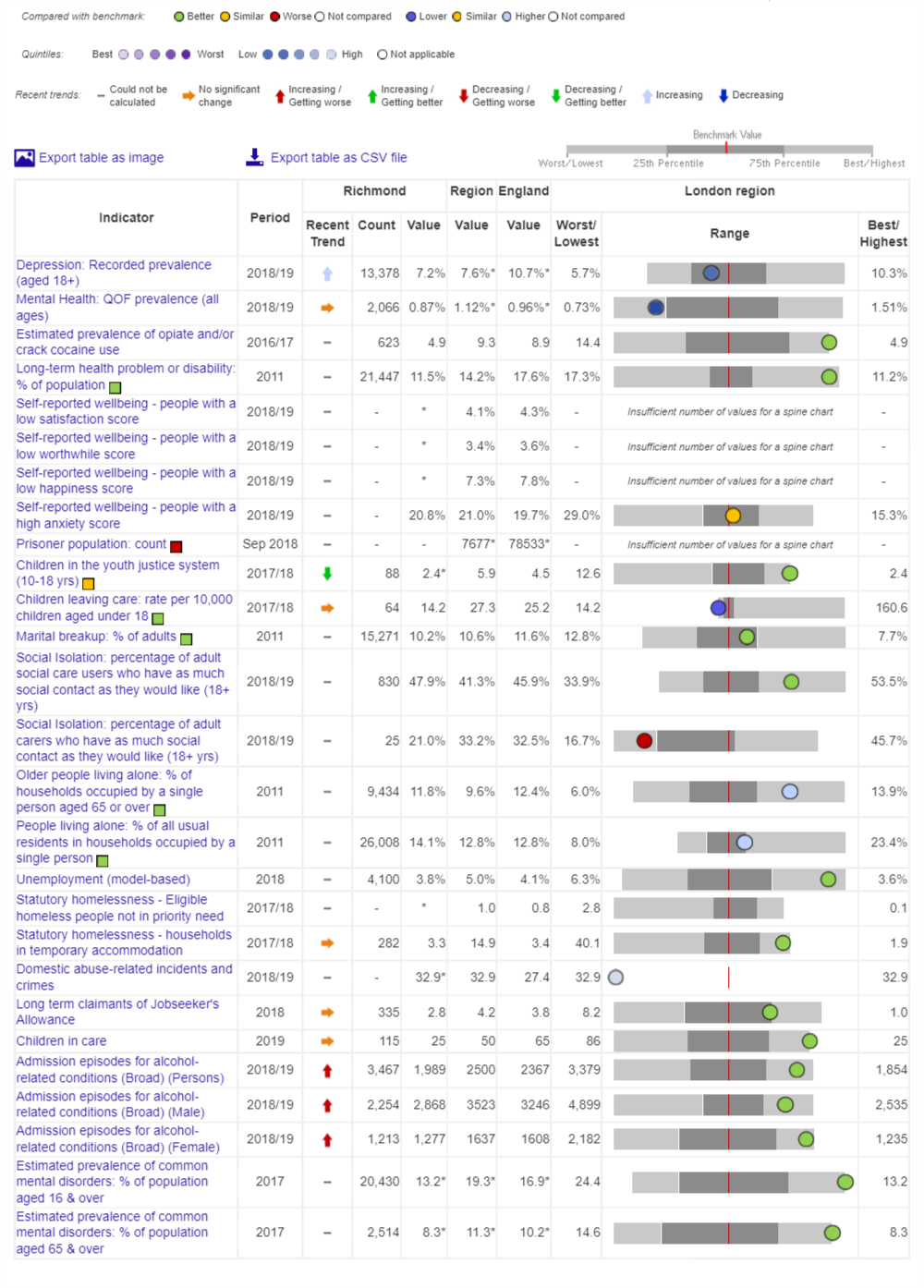
The table below can be used to see how Richmond compares to London on several measures and risk factors associated with suicide. (Public Health England, 2020)
1.2 What is the Scale of the Problem?
1.2.1
Every suicide is both an individual tragedy and a terrible loss to society, it affects a number of people directly and often many others indirectly. The impact can be devastating –psychologically, economically, and spiritually – for all those affected. Suicides can be prevented, mainly by having a society that is caring and compassionate, that supports people at times of personal crisis and ensures that marginalised individuals are helped.
1.2.2
There are a wide range of local stakeholders that have a role to play in preventing suicide. Many people who die by suicide have not been in touch with mental health services. There are many things we can do in our communities and outside hospital and care settings to help those who think suicide is their only option.
1.2.3
Suicide is a major issue for society and a leading cause of years of life lost. Although the number of people who take their own lives in England has followed a downward trend over the last 30 years, the suicide rate in England is currently 10.1 per 100,000 compared to 8.2 per 100,000 in London. The suicide rate in Richmond, 9.2 per 100,000, remains below the England average but is higher than the London average this rate equates to 10–15 suicides per year.
1.2.4
Figure 2: Number of suicides and death due to injury of undetermined intent in Richmond by gender, all ages (3 year average).
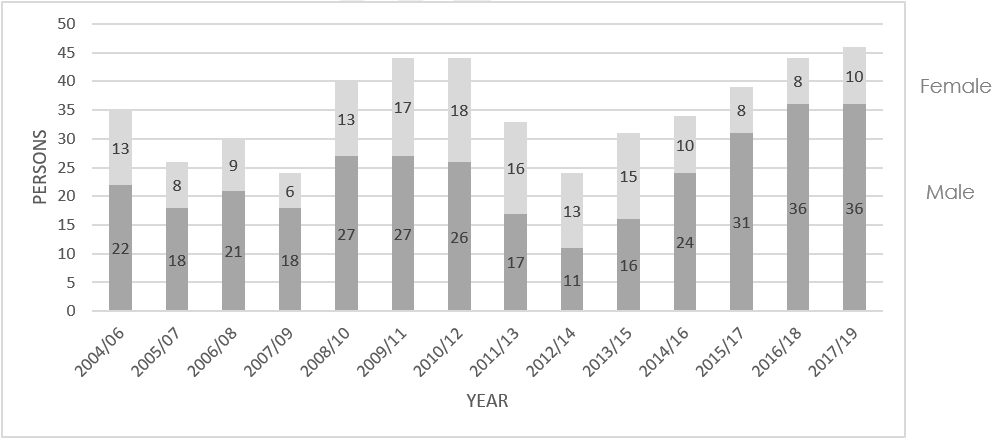
Source: Public Health England. 2020. Suicide Prevention Profile.
1.3 Self-Harm
1.3.1
Self-harm is when somebody intentionally damages or injures their body. It’s usually a way of coping with or expressing overwhelming emotional distress. More than half of people who die by suicide have a history of self-harm. Although some people who self-harm are at a high risk of suicide, most people who self-harm do not want to end their life. Self-harm is a risk factor for suicide and provides an important indicator to inform preventative interventions. A recent commentary of suicide prevention research concluded that effective interventions for reducing self‐harm in both adolescents and the adult population remains our most effective tool in preventing suicide (Sedgwick and Ougrin, 2019)[1].
1.3.2
Since 2011, hospital admissions for self-harm in young people aged 10–24 are consistently higher than the London average. The most recent data (2016/17) identifies that Richmond has the highest rate of self-harm (10–24) in London at 433.6 per 100,000, this equates to 116 individuals per year.
1.3.3
In 2014 public health carried out a Self-Harm Audit. During 2012/13–2013/14, self-harm accounted for 0.4% of A&E attendances and 1.1% of hospital admissions. The majority of self-harm admissions were due to self-poisoning (92%) and 6% were recorded as self-harm by a sharp object. The highest numbers and rates of both self-harm related A&E attendances and hospital admissions were in females age 15–24, although males aged 20–24 also experienced relatively high rates of self-harm admissions. A smaller peak was identified in females aged 50–54 for A&E attendances. There is some evidence that the white British ethnic group made up a greater than expected proportion of self-harm attendances and admissions.
1.3.4
Home was the location of the incident leading to most self-harm hospital admissions (87%). Relatively high numbers of self-harm A&E attendances and hospital admissions came from North Sheen/South Kew and Whitton areas and relatively low numbers came from the area of St. Margaret’s and East Twickenham. Eleven per cent of people attending A&E for deliberate self-harm left without receiving treatment. Comparing the number of admissions from A&E to hospital for self-harm between the two datasets suggests self-harm is particularly under-recorded in A&E.
[1] Sedgwick,R., Ougrin, D., (2019). No better than chance? Developments in predicting adolescent suicide, a commentary on Mars et al. (2018) and Beckman et al. (2018). The Journal of Child Psychology and Psychiatry, Volume 60, Issue 1 January 2019.
1.4 Suicide Audit 2014
1.4.1
Deaths included in the 2014 audit include those given a verdict of suicide, open and narrative (including some drug related deaths) by the Coroner. Statistics on causes of death produced by the Office for National Statistics (ONS) are based on the information provided at death registration. These statistics are provided to the Department of Health on an annual basis. Open verdicts are generally coded by the ONS as deaths from injury or poisoning of undetermined intent. When national statistics are presented, suicides and deaths of undetermined intent are combined. This reflects research studies which show that the majority of open verdicts are most likely suicides, although they do not meet the high legal standard of evidence required for a Coroner to record a suicide verdict. Therefore, official suicide rates are measured using this broader definition and are reflected in this suicide prevention strategy.
1.4.2
A Suicide audit provides intelligence to inform strategic priorities. Results from the Richmond Suicide audit further confirm this. Audits are time consuming requiring detailed interrogation and close working with the Coroner. We are currently exploring opportunities to develop real-time data collection which will reduce the need for resource intensive retrospective audits in the future. Thrive London are in the process of piloting a real time pan-London database to quickly identify suspected suicides. We propose to utilise this database to improve our surveillance of local suicides. In the interim the 2014 audit combined with national findings will inform the ongoing development of the strategy.
1.4.3
According to the Primary Care Mortality Database extract supplied by NHS Digital, between 2006 and 2013, 94 suicides (death due to intentional self-harm or poisoning/injury of undetermined intent) in Richmond residents were registered; an average of 12 per year
1.4.4
- Thirty-seven (39%) of the suicides registered between 2006 and 2013 in Richmond were in females and 57 (61%) were in males. This is more equal than may be expected: nationally, males account for about three quarters of all suicides.
- Over half the deaths (52%) occurred in the 35–54-year-old age group.
- One-third of suicides were due to poisoning, 31% were due to hanging, strangulation and suffocation and 36% were due to other methods
- The most common marital status for those included in the audit was single, at 40% of the total.
- The single commonest living situation for those included in the audit was living alone (32%).
- The single most common employment status was employed (30%) followed by retired (22%), unemployed (18%) and not known (12%).
- A physical health problem was recorded in 51% of cases and there was no significant difference in men (52%) and women (50%).
- Three-quarters of the cohort were recorded as having any history of mental illness. Women were slightly more likely to have been recorded as having problems with mental health than men (77% versus 72%).
- In total, 39% of all cases were recorded as having a history of previous self-harm. Men were more likely to have a history of self-harm than women (43% versus 34%)
- 42% of cases in the audit had a history of problems with alcohol. Men were significantly more likely to have had problems with alcohol than women (56% versus 23%).
- 27% of cases were reported to have had a history of substance misuse. Men had higher rates of substance misuse than women (34% versus 16%).
- 15% of cases were explicitly recorded as having financial difficulties at the time of death.
- Over a fifth (22%) of cases were found to have had relationship difficulties at the time of death.
- 27% of individuals included in this audit had experience of violence, excluding a history of self-harm or violence to oneself. Men were more likely to have been recorded as having experienced violence (30% versus 23% of women).
- Sixteen per cent of individuals included in the audit had a recorded history of criminal offence, incarceration, probation service involvement or were suspects in a criminal investigation. The proportion was much higher in males (25%) than females (5%)
1.5 Suicide Prevention Framework
1.5.1
T he framework was developed in 2015 and sets out priorities across six key areas It takes account of the evidence about what measures are likely to be effective for reducing suicide and self-harm, (including the National Institute for Health and Care Excellence guidance) and key elements have been included in the action plan included in this strategy .The framework was developed based upon discussions at a multi-agency workshop (September 2014) involving those working in mental health, community safety, substance misuse, social care, primary care, and children’s services and also a number of service users and representatives.
1.5.2
Six priority areas:
- Reduce the risk of suicide in key high-risk groups
- Tailor approaches to improve mental health among specific groups
- Prevent self-harm among young people
- Reduce access to the means of suicide
- Provide better information and support to those bereaved or affected by suicide
- support research, data collection and monitoring
1.5.3
The Suicide Prevention Framework 2015 provides a solid foundation to inform the next stage of our local strategy. The priorities outlined above are aligned to the national strategy and are consistent with the strategic objectives set out in this strategy. In many ways this strategy provides an evolution of the earlier framework and includes updated recommendations from the national strategy.
2. Where do we want to be?
2.1 Vision
Our vision is that Richmond will be a home to communities that are described as happy, thriving and resilient.
We believe that with the right support at the right time, people can recover from psychological distress and mental disorder.
We believe suicide is preventable and aim to ensure individuals;
- value their own life and the lives of others
- should never feel that suicide is the only option
- are supported in times of need, by safe, integrated, and compassionate services
2.2 Aim
The overall aim of this strategy is to reduce the rate of suicide, suicidal behaviour and self-harm through the following objectives:
2.3 Objectives
This strategy aims to:
- Improve understanding of local need – Suicide audit, pathway mapping and needs assessment
- Challenge the stigma and discrimination associated with mental disorder by:
- Increasing awareness of mental health and mental disorder
- Adopt more sensitive media reporting in relation to mental disorder, self-harm and suicide
- Improve access to information and ‘Postvention’ support – for those concerned or affected by suicide
- Prevent self-harm amongst young people – Support the development of the CAMHS Local Transformation Plan including prevention in schools, effective care pathways and A&E liaison services
- Improve access to services – Increase the numbers of people from high risk groups accessing appropriate services
- Improve crisis responses and pathways – Improvements in crisis care pathways and closer integration of mental health and substance misuse services, safer discharge, improved crisis planning.
2.4 Outcomes
- Reduction in suicides – maintain a suicide rate below the London average
- Positive experience of care
- Increased use of safety planning in key services
- Recovery and staying well
2.5 Enablers
- A multi-agency partnership approach to deliver a defined action plan (Crisis Care Concordat)
- Feedback and consultation with stakeholders
- Focus on primary and secondary prevention
- Clinical Commissioning support for Strategic Actions
- Seamless and integrated primary / secondary care pathways
- Focus on local intelligence gathering and surveillance
2.6 Guiding Principles
All activities undertaken as part of this strategy should be guided by the following principles:
| Principle | Description |
| Equity and Equality | Provision of services should be proportional to need to avoid increasing health inequalities and targeted to areas that need them the most. |
| Accessibility | Services should be accessible to all, with factors including, geography, opening hours and access for people with disabilities considered. |
| Early Intervention and Prevention | People will receive information, opportunities and support to help them take care of their own health and wellbeing, prevent deterioration and lead independent lives. |
| Integration | Service provision and care pathways should be integrated, with all relevant providers working together. This will maximise the benefits of delivery |
| Effectiveness | Services should be evidence-based and provide values for money |
| Quality | Services and activities commissioned will be of high quality, with quality and patient/ resident playing a key role in the assessment of what makes a ‘good’ service. The delivering of quality services will be a high-profile factor in the commissioning process. |
| Sustainability | Services should be developed and delivered with consideration of social, economic and environmental sustainability. |
| Safeguarding | People health and social care services will be safeguarded, throughout their experience. |
| Dignity and Respect | All people who use or encounter services will be treated with dignity and respect, recognising that people are often going through difficult times. |
2.7 Approach
The Richmond Crisis Care Concordat (CCC) was formed in 2016 and provides a multi-agency forum to lead on improved crisis care for people experiencing psychological distress. The development and implementation of the strategy and action plan will be the responsibility of this group. Key partners in the delivery of this strategy are; Richmond upon Thames Borough Council, Achieving for Children, Richmond Clinical Commissioning Group, Primary Care, South West London & St. George’s Mental Health Trust, East London Foundation Health Trust, Metropolitan Police, service users, families/carers, communities and the voluntary sector.
2.8 Risk Factors/ Groups
| Risk Groups | Risk Factors | Additional Risk factors | Mental Health Conditions[2] |
| Young and middle-aged men | Life History; Trauma in childhood; history of sexual or physical abuse; history of parental neglect | Being gay, lesbian or transgender, arising from the prejudice these groups often face | Severe depression; People with severe depression are much more likely to attempt suicide than the general population |
| People in the care of mental health services | Mental health; developing a serious mental health condition | Being in debt | Bipolar disorder; About one in three people with bipolar disorder will attempt suicide at least once. People with bipolar disorder are 20 times more likely to attempt suicide than the general population |
| History of self-harm and suicide | Drugs or alcohol misuse | Being homeless | Schizophrenia; It is estimated that 1 in 20 people with schizophrenia will take their own life. |
| People in the criminal justice system | Employment; poor job security, low levels of job satisfaction or being unemployed | Being a war veteran | Borderline personality disorder; It is estimated that just over half of people with borderline personality disorder will make at least one suicide attempt. |
| Specific occupational groups including doctors, veterinary workers, farmers and agricultural workers | Stressful life event; Bereavement, separation long term / terminal health condition | Being in prison or recently released from prison | Anorexia nervosa; It is estimated that around one in five people with anorexia will make at least one suicide attempt. |
| Genetics and Family history | Occupations that provide access to potential ways of dying by suicide e.g. working as a doctor, nurse, pharmacist, farmer or as a member of the armed forces |
[2] NHS Choices, http://www.nhs.uk/Conditions/Suicide/Pages/Causes.aspx
2.9 Confidential Enquiry into Suicide by Children and Young People
2.9.1
The purpose of a confidential enquiry is to detect areas of deficiency in clinical practice and devise recommendations to resolve them. During 2014 and 2015, 922 suicides by people aged under 25 in England and Wales were examined.
The enquiry found:
- The number of suicides at each age rose steadily in the late teens and early 20s.
- Most of those who died were male (76%), and the male to female difference was greater in those over 20.
- Academic pressures and bullying were more common before suicide in under 20s, while workplace, housing and financial problems occurred more often in 20–24 year olds.
2.9.2
The following themes were identified in the national report;
- Bereavement was common in both age groups, 25% of under 20s and 28% of 20–24 year olds, equivalent to around 125 deaths per year.
- Suicide bereavement was more common in the under 20s (11% v 6%)
- University and college students accounted for 21% of under 20s and 14% of 20–24 year olds. Only 12% were reported to be seeing student counselling services.
- Looked After Children accounted for 9% of under 20s who died with high rates of housing problems and suicidal ideation, one third of the cohort were not in recent contact with mental health care.
- LGBT young people accounted for 6% of under 20s and 3% of 20–24 year olds; a quarter of LGBT under 20 had been bullied; most had previously self-harmed.
- Suicide related internet use was implicated in 26% of deaths in under 20s, and 13% of deaths in 20–24 year olds
- Self-harm was reported in 52% of under 20s and 41% of 20–24 year olds who died. Around 60% in both age groups were known to services and around 40% had been in recent contact—in only 26% this was mental health care.
- Interagency collaboration was variable and risk recognition appeared poor.
2.9.3
The following key messages were identified in the report;
- Suicide in young people is rarely caused by one thing; it usually follows a combination of previous vulnerability and recent events.
- The stresses identified that lead to suicide are common in young people; most come through them without serious harm.
- Important themes for suicide prevention are support for or management of family factors childhood abuse, bullying, physical health, social isolation, mental ill-health and alcohol or drug misuse.
- Specific actions are needed for the following groups (1) support for young people who are bereaved, especially by suicide (2) greater priority for mental health in colleges and universities (3) housing and mental health care for looked after children (4) mental health support for LGBT young people.
- Further efforts are needed to remove information on suicide methods from the internet; and to encourage online safety, especially for under 20s.
- Suicide prevention in children and young people is a role shared by front-line agencies; they need to improve access, collaboration and risk management skills.
- Services which respond to self-harm are key to suicide prevention in children and young people and should work with services for alcohol and drug misuse, factors that are linked to subsequent suicide.
2.10 Community Action Plan
2.10.1
During 2018, a task group, led by public health, was set up to formulate a Community Action Plan to mitigate against the risk of Suicide Clusters and contagion. A small multi-agency group created the plan based upon a practice resource developed by Public Health England.
2.10.2
The term “suicide cluster” describes a situation in which more suicides than expected occur in terms of time, local, or both. A suicide cluster usually includes three or more deaths. With suicidal behaviour increasingly spreading via the internet and social media, a greater number of suicides than expected may well occur in a specific time period and be spread out geographically (so called mass clusters).
2.10.3
Suicide clusters understandably cause great concern and may lead to hasty responses. It is important that plans for such occurrences are prepared in advance, to ensure a measured and effective response. With this in mind the Richmond Suicide Community Action Plan provides a systematic process to identify potential clusters and provide a series of swift interventions to mitigate the threat.
2.10.4
The Community Action Plan has two specific facets: active surveillance through a Suicide Surveillance Group and mitigation through a multi-agency Suicide Response Group. The plan has been developed with partners including Public Health, Clinical Commissioning Group, Metropolitan Police, Local Safeguarding Children Board, Adult Social Care, Achieving for Children. The Suicide Surveillance Group will meet regularly throughout the year to monitor the levels of suicide and to identify potential suicide clusters and contagion
3. How will we get there?
3.1 Strategic Objectives and Action Plan 2019/20
| Objective | Action | Measure / Outcome | Owner | Timescale |
| 1. Understand local need | 1.1 Set up a system to monitor suicide through a Suicide Surveillance Group | Quarterly meeting of the Suicide Surveillance Group | GM | Sept 19 |
| 1.2 Develop a Suicide Prevention survey for Primary Care (GPs and Practice Nurses) to ascertain levels of need related to self-harm and suicide. | Survey developed, disseminated and recommendations drafted | CCG
AD |
Mar 20 | |
| 2. Challenge stigma and Discrimination | 2.1 Distribute suicide reporting guidelines to local media groups | Media organisations identified, and guidance distributed with accompanying letter from Director Public Health | GM | Sept 19 |
| 2.2 Mental Health First Aid and Suicide Prevention Training delivered to Frontline staff and Community and Voluntary Sector | Baseline established, and annual summary of courses delivered | GM | Mar 20 | |
| 3. Improve access to Information and ‘Postvention’ support | 3.1 Support Secondary state maintained and independent schools to access suicide prevention training. | 20 Schools accessing Papyrus suicide prevention training for schools | GM | April 19 |
| 3.2 Primary Care fact sheet distributed to primary care settings (GP practices and health centres) | Primary care fact sheet distributed to GP practices and health centres | CCG
AD |
Mar 20 | |
| 3.3 Help is at hand booklets and Z cards distributed to Primary Care settings | All GP and Health Centres provided with Help is at Hand materials | CCG
AD |
Sept 19 | |
| 3.4 Suicide prevention signage at high risk locations including railway stations, bridges and level crossings | Location of additional signage reported to CCC on quarterly basis | HR | Mar 20 | |
| 4. Prevent self-harm amongst young people | 4.1 Promote whole school approach to emotional health and well-being as set out in the CAMHS LTP | Whole school approach audit implemented, and best practice seminars developed and attended by schools | CCG
DR |
Sept 19 |
| 4.2 Ensure support for young people who self-harm through locally agreed self-harm pathway | Self-harm pathway developed and disseminated to universal services | CCG
DR |
Mar 20 | |
| 5. Improve Access to local services | 5.1 Improve the Integrated support for individuals experiencing co-occurring mental health and substance misuse support | Clinical Interface meetings to receive recommendations on cases identified through the Drug and Alcohol Related Deaths Panel. | RK | Dec 19 |
| 5.2 Improve access to psychological therapies for key risk groups including men. | Key risk groups identified and KPIs agreed with commissioner and provider | CCG
AD |
Mar 20 | |
| 5.3 Develop and implement Suicide Community Action Plan to mitigate against cluster and contagion. | Community Action Plan agreed by Crisis Care Concordat and first meeting of Suicide Surveillance Group to monitor suicide data | GM | Sept 19 | |
| 5.4 Increase access to Mental Health First Aid Training and suicide prevention training for school’s staff, first responders and universal services | Baseline established, and annual summary of courses delivered. | GM | Mar 20 | |
| 6. Improve crisis responses and pathways | 6.1 Review crisis pathways across Richmond by mapping access point to treatment and supporting and ensuring co-ordinated and integrated care across primary and secondary mental health services in response to need | CCG to facilitate the crisis care mapping which will form part of the South West London crisis work.
Local task and finish group to link into the South West London Crisis work. |
CCG
AD |
Mar 20 |
| 6.2 Ensure safer hospital discharge to include follow up within 72 hours after leaving hospital. | 95% of service users leaving hospital will have a face to face review and risk assessment within 72 hrs of discharge. | CHa | Mar 20 | |
| 6.3 Review of the SWL pathways for Children and young people requiring crisis. | Healthy London Partnership to undertake a peer review of SWLSTG crisis care pathways. | CCG
DR |
Dec 19 | |
| 6.4 Effective liaison in urgent care centres and A&E. | 95% of attendances to urgent care, receiving an assessment from the Core 24 team within 1 hr.
KPI monthly monitoring |
CCG
AD |
Dec 19 |
4. How Will We Know When We’ve Got There? – Monitoring the Strategy
4.1 Governance
4.1.1
The Suicide Prevention Strategy has been agreed by the Richmond Crisis Care Concordat; The Health and Wellbeing Board and the Adult Social Services, Health and Housing Services Committee.
4.1.2
The multi-agency Richmond Crisis Care Concordat will be responsible for overseeing the progress and delivery of the action plan and will report back to the Health and Well-being Board annually.
4.2 Interdependent Action Plans
- CAMHS Transformation Plan 2018
- LSCB Young Peoples Risky Behaviour Action Plan 2018
- SWL Health and Care Partnership Plan 2019
- South West London and St. George’s Mental Health Trust Suicide Prevention Plan
4.3 Baseline Metrics 18/19 and beyond
4.3.1
The following table identifies key indicators
| Indicator | Baseline (18/19) | 19/20 |
| Suicide Rate | 7.9 Per 100,000 | 9.2 Per 100,000 |
| Emergency Hospital Admission for Intentional Self-Harm | 132.2 per 100,000 | Awaiting data update |
| Number of Richmond patients in secondary care dying by suicide | 5 | Awaiting data update |
| Adult males accessing psychological therapies | 1,313 | Awaiting data update |
| No of MHFA training sessions | 18 | Awaiting data update |
Bibliography
Cross-Government Suicide Prevention Workplan, published in January 2019 by the Department of Health and Social Care
https://www.gov.uk/government/publications/suicide-prevention-cross-government-plan
Future in mind: promoting, protecting and improving our children and young people’s mental health and wellbeing, Published by the Department of Health and NHS England in 2012
www.gov.uk/government/uploads/system/uploads/attachment_data/file/414024/Childrens_Mental_Health.pdf
Local Suicide Prevention Planning, A practice resource, Published by Public Health England in 2016
https://www.gov.uk/government/publications/suicide-prevention-developing-a-local-action-plan
Preventing Suicide in England: a cross-government outcomes strategy to save lives, Published by the department of Health in 2012
https://www.gov.uk/government/publications/suicide-prevention-strategy-for-england
Preventing suicide in England: Third progress report of the cross-government outcomes strategy to save lives, published by the Department of Health and Social Care in 2017
https://www.gov.uk/government/publications/suicide-prevention-third-annual-report
Preventing suicide in England: fourth progress report of the cross-government outcomes strategy to save lives, published by the Department of Health and Social Care in 2019
https://www.gov.uk/government/publications/suicide-prevention-fourth-annual-report
Suicide prevention: identifying and responding to suicide clusters, published by Public Health England in 2015
Crisis Care Concordat Membership
Organisations
| Richmond Clinical Commissioning Group |
| Achieving for Children |
| East London Foundation Trust |
| LBRuT (Adult Social Services) |
| LBRuT (Public Health) |
| LBRuT (Housing) |
| LBRuT (Safeguarding Adults Team) |
| Richmond GPs |
| Richmond Mind |
| London Ambulance Service |
| SW London Health and Care Partnership |
| Metroplitan Police |
| British Transport Police |
| Network Rail |
| South West Trains |
| Comfort Care/ Retreat Crisis House |
| SWLStG Mental Health Trust |
| SPEAR |
| Child and Adolescent Mental Health Services |
| Substance Misuse Services (CGL) |
