Introduction
Aim
The purpose of this document is to scope and review cardiology services for Richmond patients. It aims to understand current clinical practice and referral routes for specific cardiology services and conditions, including diagnostics, and paediatric diagnostics. It sets out the local needs, costs, and makes the case for change for improving cardiology services for Richmond patients. The latest guidance, evidence, and best practice have been referenced and incorporated. Recommendations have been put forward to develop cost effective, equitable, and accessible high quality services for our patients.
Who is this for?
A cardiology pathway steering stakeholder group was set up to lead the review with a smaller project working group to identify, understand and map existing services, identify gaps in service provision, identify patient need, define best practice and drive quality and cost efficiencies through service redesign. Both groups were multi-disciplinary, comprising of clinicians from primary and secondary care, commissioners, and public health professionals. The project has been led, coordinated and supported by the Public Health department, with a dedicated public health lead working full time on the pathway review and redesign work.
The steering group met monthly over a 10 month period who delivered a final presentation at the Clinical Advisory Group on 4th March 2014. A smaller project team was set up to undertake the work and met fortnightly. See Appendix 1 for the membership list for the projects team and steering group.
Background
Cardiac Conditions
There are a number of cardiac conditions that a patient can be born with, or may develop over time due to a number of reasons, including:
- Rheumatic heart disease (Valvular heart disease)
- Hypertensive heart disease:
- Aneurysms
- High blood pressure
- Ischaemic heart disease (IHD) also known as Coronary Heart Disease (CHD) – this is caused by the narrowing of the coronary arteries, leading to a decrease of blood supply to the heart.
- Angina
- Inflammatory heart disease:
- Cardiomyopathy
- Pericardial disease
- Congenital heart disease – this term covers various heart defects an individual is born with.
- Heart failure (HF)
- Cerebrovascular heart disease – this is the blood vessels in the brain; blood supply to a part of the brain has been hindered, which causes this disease (TO BE COVERED IN PART 2 OF THE REVIEW).
- Stroke
- Transient ischemic attack (TIA)
- Cardiac Arrhythmias – this is irregularities in the heart beat; either beating too slow or too fast.
- Atrial Fibrillation (AF) (TO BE COVERED IN PART 2 OF THE REVIEW)
- Palpitations
- Heart block
- Brachycardias
- Tachycardias
- Ventricular fibrillation
- Long QT syndrome
- Wolff Parkinson White syndrome
Evidence Based Practice
Evidence based practice in health and social care is essential in order to have an integrated approach to deliver the most clinically appropriate, high-quality and safe care by using a combination of current evidence, clinical research, guidelines and policies.
The National Service Framework for Coronary Heart Disease (Department of Health, March 2000).This NSF sets out twelve service standards that cover the following areas:
- Reducing heart disease in the population
- Preventing CHD in high-risk patients
- Heart attack and other acute coronary syndromes
- Stable angina
- Revascularisation
- Heart failure
The National Institute of Health and Clinical Excellence (NICE) have published a number of documents with guidance to reflect good practice at key stages of diagnosis, management and further care for various heart conditions, including:
- NICE Chest pain of recent onset (2010)
- NICE Prevention of cardiovascular disease (2010)
- NICE Unstable angina and NSTEMI (2010)
- NICE TA Implantable cardioverter defibrillators for arrhythmias (2007)
- NCCPC Lipid modification (2010)
- NICE PH25 Prevention of cardiovascular disease (2010)
- MI: secondary prevention in primary and secondary care for patients following a myocardial infarction. (2007)
A number of other professional bodies, organisations and charities have published credible guidelines for the identification, treatment and management of heart diseases including:
- Scottish Intercollegiate Guidelines Network (SIGN) Acute Coronary Syndromes (2012).
- The Health Foundation. Healthcare delivery models for prevention of cardiovascular disease (CVD)
Although a wide range of clinical guidance exists for the plethora of heart conditions, there does not appear to be an agreed guide for the general initial investigation of suspected cardiology conditions. However, using a combination of key clinical guidance and primary literature, knowledge can be drawn to determine key best practice methods and diagnostic procedures to identify and investigate a suspected cardiology condition.
Best Practice for cardiology/suspected cardiology at primary care presentation
Best practice guidelines for initially assessing, identifying and managing patients for the common cardiology conditions GPs usually see at primary care.
There are a number of symptoms a patient may present with that is indicative of a cardiology condition. Several symptoms can appear together, or only one may be present at the time of GP presentation[i],[ii],[iii],[iv]:
- Chest pain/discomfort
- Dull pain, ache or ‘heavy’ feeling in chest
- discomfort in the neck, shoulders, jaw, or arms
- Difficulty breathing during regular activities and rest
- Palpitations or heart flutters
- syncope
- dizziness
- sweatiness
- breathlessness/ shortness of breath
- headaches
- transient visual loss
- wheeze
- High BP
- Unexplained indigestion, belching, epigastric pain
- nausea/vomiting,
- back or jaw pain,
- loss of appetite or heartburn,
- tiredness or weakness,
- coughing
As well as assessing the signs and symptoms of a patient, it is essential that the GP takes the history of the patient and identifies any risk factors that would influence the risk of an individual having a heart condition including, but not limited to[v]:
- Diabetes
- Hypertension
- Hyperlipidemia
- Smoking
- Obesity
- High cholesterol
- Physical inactivity
- Age
- Family history
Acute coronary syndrome (ACS)
ACS is the term used when referring to the family of unstable coronary artery diseases (CAD) ranging from unstable angina to transmural myocardial infarction (MI)[vi] . Most of these diseases have similar aetiology. When a GP suspects a patient may have any of the conditions under ACS, the following should be done[vii],[viii]:
- Take patient history
- Clinical examination (see table 1)
- Assess if patient has any of the risk factors for ACS/CVD and other heart conditions
- 12-lead ECG – this can be repeated if there is diagnostic uncertainty or change in the patient’s clinical status
When suspecting CAD, but it is not confirmed and stable angina is nether diagnosed or excluded, the GP should estimate the likelihood of the patient having CAD which can be done using table 2[ix].
Angina (see appendix 4 for pathway)
Angina is a pain or discomfort in the chest usually caused by CAD; however in some cases the pain may affect some people only in the arm, neck, stomach or jaw[x]. Types of angina include:
- Stable Angina – Constricting discomfort in the front of the chest, in the neck, shoulders, jaw, or arms. It is usually precipitated by physical exertion; the pain usually lasts only for a few minutes.
- Unstable angina (symptoms can manifest in both stable or unstable)– dull/heavy to sharp chest pain or discomfort
- Constricting discomfort or pain in the front of the chest, in the neck, shoulders, jaw, or arms.
For patients with suspected cardiac chest pain, they should be referred to a rapid access chest pain clinic (RACPC).
Unstable angina
When a patient presents with acute chest pain the GP should[xi]:
- Take a resting ECG ASAP – do not exclude an acute coronary syndrome (ACS) or assess ACS differently in ethnic groups.
- Monitor oxygen saturation (SpO2) using pulse oxiemtry. Only offer oxygen to people with SpO2 less than 94% who are not at risk of hypercapnic respiratory failure (aim for SpO2 of 94–98%) and people with COPD and at risk of hypercapnic respiratory failure( aim to achieve SpO2 of 88–92% until blood gas analysis is available).
Diagnosis of stable angina
If a patient presents, do the following:
- Clinical assessment – history and examination (see table 1)
- Clinical assessment and a resting 12-lead ECG ( NB a normal resting 12-lead ECG does not exclude stable angina as a diagnosis)
Once angina has been diagnosed as stable, it can be managed effectively within primary care. For presentation and management of stable angina in primary care (see appendix 4 for pathway).
Figure 1 Clinical history and physical examinations that should be performed for patients with suspected or confirmed stable angina
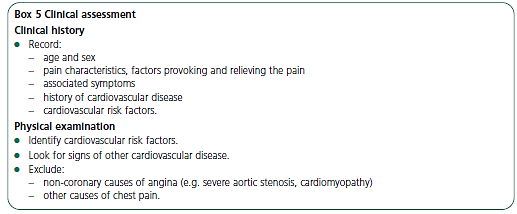
Source: NICE Chest pain of recent ofset (2010)
Coronary Heart Disease (CHD) (also known as Coronary Artery Disease (CAD))
CHD/CAD is the blockage of the bold vessel and Ischaemic Heart Disease (IHD) happens due to the insufficient blood flow to the muscles through the coronary arteries. Angina is usually an indication of CHD.
Table 1 Reference for people estimated to have CAD according to certain factors
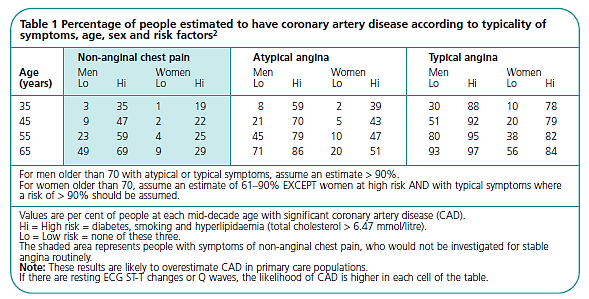
Source: NICE Chest pain of recent onset (2010)
Table 2 Probability table to decide how to refer suspected CAD patients.
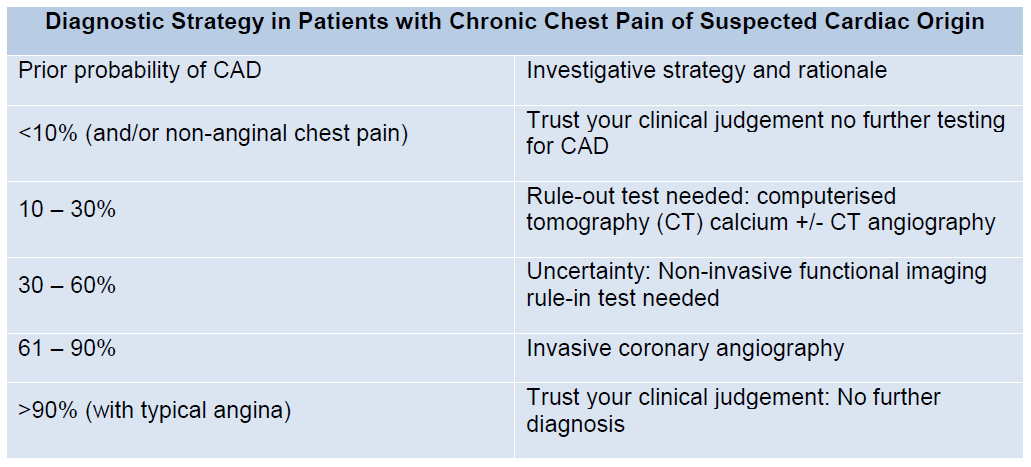
Source: Greater Manchester and Cheshire Cardiac and Stroke Network Primary Care Pathways
Both tables should help the GP decide whether to refer patients to the cardiology department.
Hypertension
Hypertension is arguably the most important modifiable risk factor for CHD (the leading cause of premature death in the UK). It is also an important cause of congestive heart failure[xii]. In England, 32% of men and 30% of women aged 16 years or over have hypertension (persistent raised blood pressure of 140/90mmHg or above) or are being treated for high blood pressure (BP)[xiii]. This means that, in terms of the average GP’s list of 2,000 patients, about 500 will have hypertension[xiv]. The strong association in the UK between increasing age and increasing systolic BP is thought to reflect the length of time that people have been exposed to modifiable lifestyle risk factors.
N.B. The thresholds for hypertension in people with Type 1 or Type 2 diabetes are slightly lower.
If a patient has a BP of 140/90 mmHg or higher, the GP should do the following[xv] as per the NICE guidance:
- Offer ambulatory blood pressure monitoring (ABPM) to confirm the diagnosis of hypertension
- When using ABPM to confirm diagnosis, ensure that at least two measurements per hour are taken during the person’s usual waking hours (average of 14 measurements during waking hours)
- When using home blood pressure monitoring (HBPM) to confirm a diagnosis of hypertension, ensure that:
- For each BP recording, two consecutive measurements are taken, at least 1 minute apart and with the person seated, and
- BP is recorded twice daily, ideally in the morning and evening and
- BP recording continues for at least 4 days, ideally for 7 days.
- NB: Discard the measurements taken on the first day and use the average value of all the remaining measurements to confirm a diagnosis of hypertension.
Whilst waiting to confirm the diagnosis of suspected hypertension, GPs should carry out investigations for target organ damage and a formal assessment of CVD risk:
- Use estimation of CVD risk to discuss prognosis and healthcare options with people with hypertension
- Assess target organ damage:
- Test for protein in the urine (albumin: creatinine ratio) and test for haematuria.
- Take blood sample to measure plasma glucose, electrolytes, creatinine, estimated glomerular filtration rate (eGFR), serum total cholesterol and HDL cholesterol.
- Examine the fundi for the presence of hypertensive retinopathy.
- Arrange for a 12-lead ECG.
Refer people to specialist care on the same day if they present with:
- Accelerated hypertension (BP higher than 180/110 mmHg) with signs of papilloedema and/or retinal haemorrhage, or
- Suspected phaeochromocytoma (labile or postural hypotension, headache, palpitations, pallor and diaphoresis).
- People with signs and symptoms suggesting a secondary cause of hypertension.
Cardiovascular disease (CVD) risk and prevention
CVD is a major public health problem as it known to be the leading cause of death in England[xvi],[xvii]. CVD predominantly affects people aged 50 and over; therefore making age the main determinant of CVD risk. The other main determinants of CVD risk are smoking, raised BP and raised cholesterol levels; the risk of CVD increases even more when these factors are combined. These factors account of 80% of all premature CHD[xviii].
QRISK®2 is a CVD risk score which is designed to identify people at high risk of developing CVD who need to be recalled and assessed in more detail to reduce their risk of developing CVD. The QRISK®2 score estimates the risk of a person developing CVD over the next 10 years. 10 year risk of CVD means the risk of someone developing CVD over the next ten years. If someone has a 10 year QRISK®2 score of 20% then they have a ‘one in five’ chance of getting CVD over the next 10 years. Incorporating ethnicity, deprivation, and other clinical conditions into the QRISK2 algorithm for risk of CVD improves the accuracy of identification of those at high risk in a nationally representative population[xix]
NICE are currently in the process of reviewing and updating their guidelines for Cardiovascular risk assessment and modification of blood lipids for the primary and secondary prevention of CVD. The draft for consultation indicates that the threshold for offering statin treatment will be reduced from 20% to people with a 10% risk of developing CVD over the next 10 years. Furthermore, the recommended first line choice of statin has changed from simvastatin to atorvastatin.[xx] Further planning will be required to implement the changes in NICE guidance (once finalised); implications on local resource will have to be considered at this time.
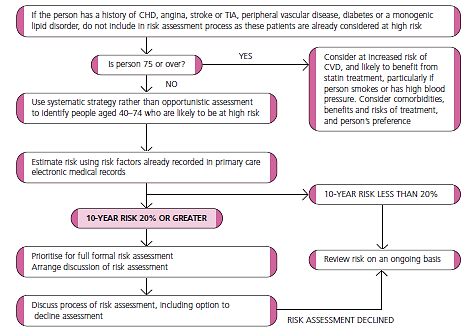
Below is an algorithm from NICE (figure 1) describing the process in performing a formal CVD risk assessment for patients (See NICE CVD risk prevention for full guidance on prevention and management of CVD risk).
Figure 2 Full formal CVD risk assessment
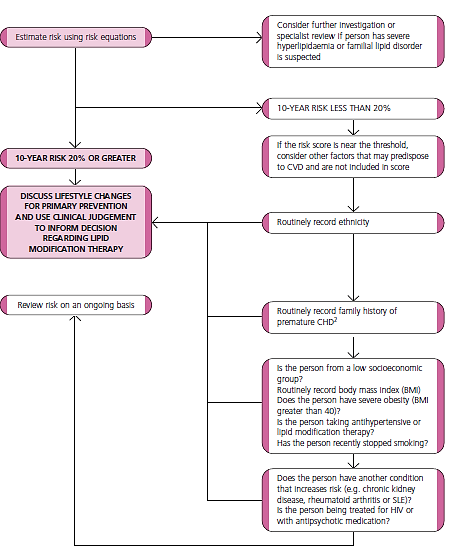
Source: NICE Lipid modification (2010)
Palpitations
The term palpitation can be used any time a patient complains of an abnormal awareness of their heart beat.
High risk factors to be aware of:
- History of pre-syncope/syncope
- Exertional cardiac symptoms
- Pre-existing heart disease ( HF, IHD, valvular and congenital heart disease)
From clinical guidance and literature referring to the diagnosis and management of palpitations, it would appear that the primary investigatory test that should be conducted to for a patient with suspected palpitations should be an ECG[xxi][xxii].
Arrhythmias
Palpitations and cardiac arrhythmias in patients are relatively common and the majority of these patients should be managed in primary care[xxiii]. A recent study in the UK demonstrated that a large number of patients with palpitations and arrhythmia symptoms did not require referral to cardiology services in secondary care and significant resources are dedicated to these low risk patients. By using a GP direct access BP holter and event monitoring service, the results showed that 96.2% of patients did not require referral to cardiology clinic and no reported adverse events[xxiv]. The monitoring of the heart’s rhythms is pivotal to the diagnosis of cardiac arrhythmias. There are various types of arrhythmias and they can be detected by using different ways to monitor the heart’s rhythm under different conditions within primary care without having to undergo a formal review at a cardiology clinic:
- ECG/24 hr ECG – this can be used to confirm ectopic beats – early (premature) or extra heartbeats that can cause palpitations [xxv]
- Exercise Tolerance Test (ETT)
- Cardiac event recorder – this can be used if arrhythmia does not occur often
- Echo – this should be able to show if there are any problems with the heart muscles or heart valves.
- Electrophysiological (EP) testing – the patient must be referred to a cardiologist for this test to be conducted
The Resuscitation Council (UK) recommends strongly a policy of attempting defibrillation with the minimum of delay in victims of ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) cardiac arrest[xxvi] (both conditions are cardiac arrhythmias). It is recommended that automated external defibrillators (AEDs) should be available in all healthcare settings[xxvii] and all healthcare workers should also be trained, authorised and encouraged to perform defibrillation[xxviii] when necessary.
Figure 3 Primary care pathway for initial presentation of suspected palpitations
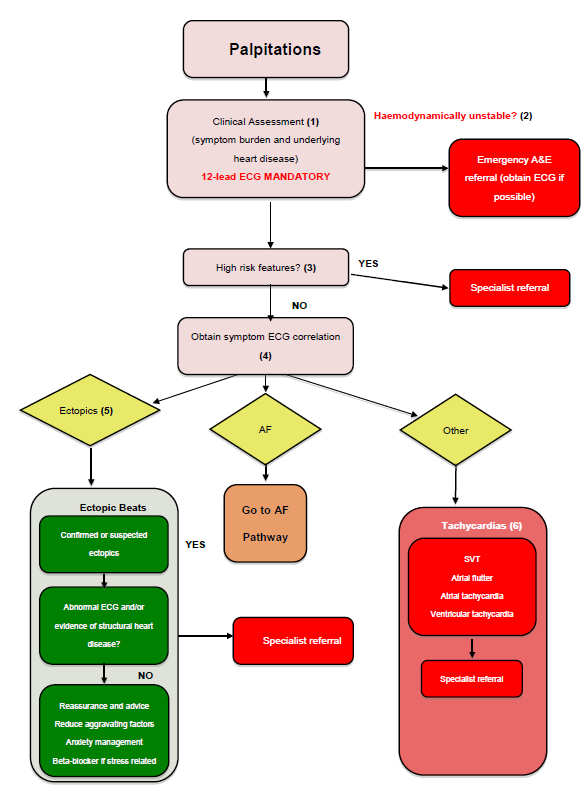
Source: Greater Manchester and Cheshire Cardiac and Stroke Network Primary Care Pathways
Primary prevention of sudden cardiac death (SCD)
SCD occurs in approximately 50,000–70,000 people annually in the UK; this is also representative of the largest proportion of the deaths attributable to CHD. Approximately 85–90% of SCD is due to the first recognised arrhythmic event; the remaining 10–15% is due to recurrent events[xxix].
Risk factors associated with SCD to be aware of, but not limited to[xxx]:
- Diabetes Mellitus
- Hypertension
- Left ventricular hypertrophy
- Hyperlipidemia
- Dietary factors
- Excessive alcohol consumption
- Physical inactivity
- Smoking
Rick factor interventions should be given to those who are at risk of CHD, including encouragement of moderate physical activity and other health promotion models[xxxi].
Heart murmurs
A heart murmur is an unexpected sound which a doctor may hear when listening to the heart with a stethoscope[xxxii]. Sometimes the murmur is caused by an underlying heart valve abnormality, but often there is no cause at all (innocent murmur).
For suspected murmurs, the GP should do the following[xxxiii]:
- Take a history and perform clinical examination ( use stethoscope to check the grade of the murmur- see table x below)
- If examination is normal, perform or refer for ECG
- If there are indications of heart disease, then refer to specialist cardiologist
- Patients with normal examinations and ECG can be referred to Direct Access Echo
- If the Echo comes back as abnormal, then refer patient to specialist.
Table 3 Intensity grades of heart murmurs
|
Grade |
Description |
|
1 |
Faint murmur that can only be heard after a few seconds have elapsed. |
|
2 |
Faint murmur that is heard immediately. |
|
3 |
Moderate murmur intensity. |
|
4 |
Loud murmur. |
|
5 |
Very loud murmur that occasionally can be heard when the stethoscope is placed only partially on the chest. |
|
6 |
Very loud murmur that can be heard when the stethoscope is off the chest entirely. |
Source: Lessard, E et al. Patient with a heart murmur. JADA, Vol.136 (2005)
Commissioning pathways
Commissioning is a vital part of the NHS healthcare system as it is there to ensure the right amount of clinical care is purchased and available for a particular population.
Below is a list of the various publications that can be used to assist services in commissioning the most appropriate, and clinically safe service for the diagnosis of patients with heart disease, or managing them effectively within the community:
- British Cardiovascular Society (BCS) (2011) Commissioning of Cardiac Services – A Resource Pack from the British Cardiovascular Society
- South West Joint Improvement Partnership (2010) A Toolkit to Support the Commissioning of Targeted Preventative Services
- Department of Health (2006) Adult congenital heart disease commissioning guide
Local Picture
Prevalence of cardiology conditions in Richmond
In Richmond, almost 32,000 of the GP registered population have a heart condition (including congestive heart failure (HF), hypertension, IHD, and AF; a rate equivalent 1,597 people with a heart condition per 100,000 in the Richmond population[xxxiv]. Coronary heart disease (CHD) is more prevalent in lower socio-economic groups and in certain ethnic minorities than the rest of the population[xxxv]. The National Service Framework (NSF) highlights that inequalities in the manifestation, detection, treatment and management of heart disease have arisen because information, services and resources are not adequately reaching those whose situations, position in society and lifestyle choices puts them at greater risk of CHD.
Out of all the boroughs in London, Richmond has the lowest SMR for people under 75 years with all types of CVDs (see figure 3). Observed improvement in the low levels of CVDs in comparison to other boroughs could be due to the weight-loss programmes within the borough, BP monitoring being conducted by GPs and CVD risk monitoring at primary care.
Figure 4 Under 75 directly age standardised mortality rate per 100,000 for all cardiovascular diseases by London Borough, 2011/12
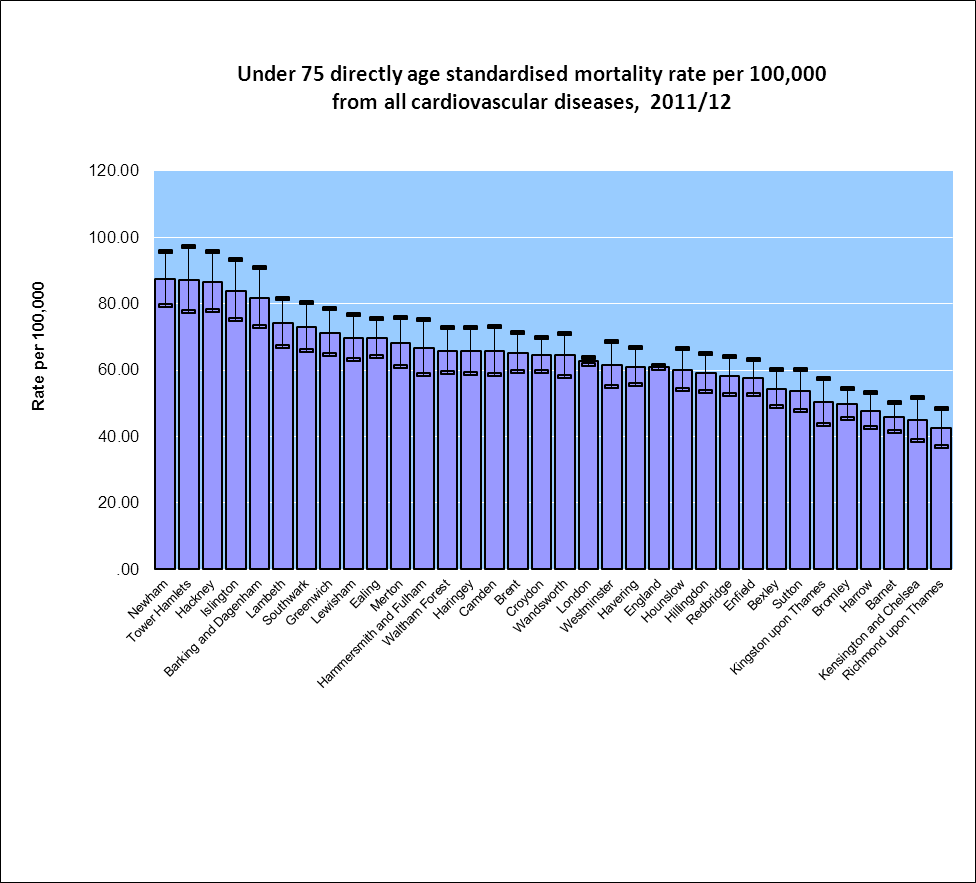
Source: LBRuT Public Health Intelligence (2013)
In Richmond, a large majority of the population (approximately 85%) of the population are White British with approximately 15% of the population from Ethnic minority backgrounds (see figure 4). Evidence has already highlighted the increased heart disease risk associated with these ethnic groups.
Figure 5 The Richmond borough percentage population by ethnicity
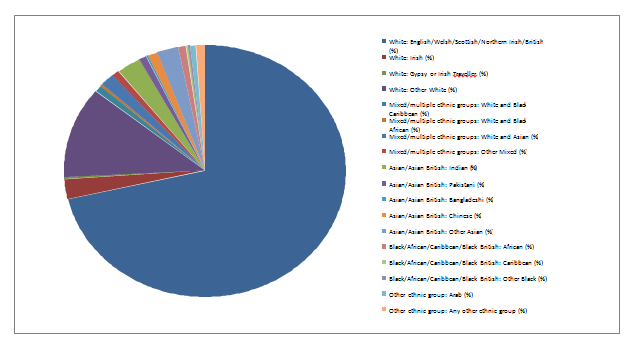
Source: LBRuT Public Health Intelligence (2013)
It is important to recognise the diversity within the LBRuT population, and the necessity to make adequate and accessible service provision for the minority groups to ensure they are aware of the services available to help prevent heart disease and/or manage an already identified heart disease. A small case study in the UK recognised there could be some benefit in identifying and managing heart disease in black and other minority community groups through having culturally adapted group sessions to raise awareness, offer medication reviews if necessary as well as BP monitoring.
Ageing population
Around 24,000 (12.6%) of the London Borough of Richmond upon Thames (LBRuT) population are aged 65 years and over, which is higher than the proportion across London (11.5%) but lower than the England average of 16.3%[xxxvi]. Richmond also has over 4000 people aged 85 and over, which is a higher proportion than London (2.08% of the borough population compared to 1.66% London-wide)[xxxvii]. The life expectancy for the Richmond population aged 65 years and over is significantly higher than London and England (23 years for women, 21 years for men)[xxxviii]. These values clearly indicate that LBRuT is more likely to have a higher proportion of older people that will require multiple health and social care needs that will impact the way local services are provided.
Approximately 6% of the 65 years + population and 2% of the 85years + population are from Black and Asian Minority Ethnic (BAME) backgrounds[xxxix]. As the number of older people in the borough is estimated to continue to increase, it is expected that the proportion of the BAME population within this age group will also increase. It is important to recognise the difference in need that exists for the ageing BAME population, as they are more vulnerable and more likely not to be utilising the borough services or face challenges when accessing cardiology services.
The more deprived wards in the borough are expected to have the largest increases in older people, which are expected between the ages of 65 to 74 years.[xl]
Co-morbidities
The key risk factors for cardiology conditions include smoking, physically inactive lifestyles, poor diet, excess salt, obesity, alcohol and diabetes. Other non-communicable diseases such as cancer, COPD, depression and dementia are also diseases closely linked with heart disease.
Figure 5 (below) shows the percentage of people with a long-term condition associated with heart disease in Richmond. Over 20% of people with heart disease in Richmond also have depression or anxiety. Over 15% of people with a heart condition in Richmond have at least three other long-term conditions, and 10% of patients have four other long-term conditions with depression and anxiety being most prevalent. This is an indication that a considerable proportion of cardiology patients in Richmond will require more than just clinical cardiology services to help them adequately manage their conditions; prompting a more integrated care approach to ensure the patient has access to all the necessary service, improving the patient experience.
Figure 6 Percentage of the Richmond population with heart disease and one or more other long-term condition.
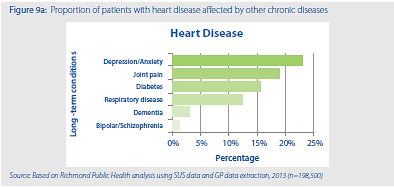
Source: London Borough of Richmond upon Thames Public Health Annual Report (2013)
Figures 6, 7, and 8 (below) show an uneven distribution of heart disease within the borough. The graphs show that the highest proportion of GP registered patients on the CHD, hypertension and CVD register are situated in Twickenham and Whitton, comprising of some of the most deprived areas within the borough, demonstrating that heart disease is more prevalent in the deprived areas. It also has the highest population in the borough in comparison with the other LBRuT clinical networks within the borough. It is therefore necessary to review the cardiology services that residents in this area access the most to assess if the current services are appropriate and adequate to prevent and manage heart diseases effectively.
Figure 7 Proportion of GP list size on the coronary heart disease (CHD) register by practice (by locality)
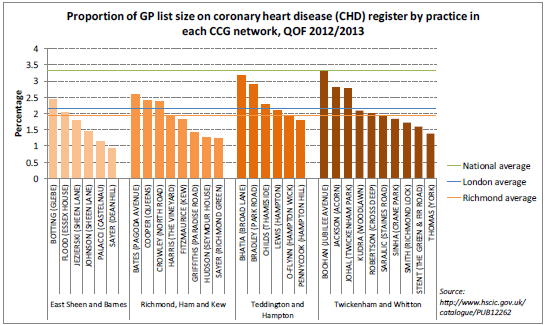
Source: Richmond CCG Clinical Network Data Pack (2013)
Figure 8 Proportion of GP list size on the hypertension register by practice (by locality)
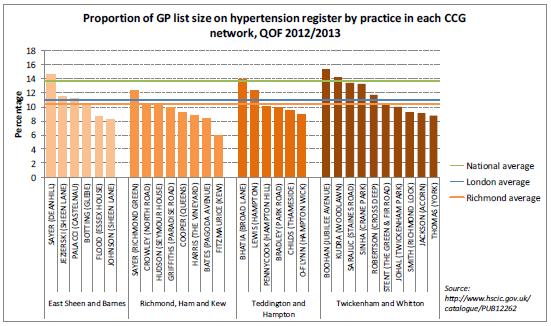
Source: Richmond CCG Clinical Network Data Pack (2013)
Figure 9 Proportion of GP list size on the cardiovascular disease (CVD) risk prevention register by practice (by locality)
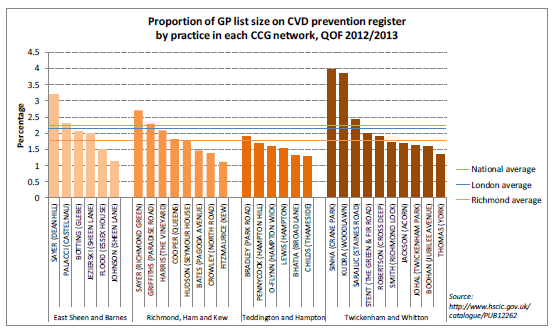
Source: Richmond CCG Clinical Network Data Pack (2013)
The closest cardiology services to the Twickenham and Whitton residents are the community cardiology service run by Imperial College Hospitals Trust (ICHT) at Teddington Memorial Hospital (TMH) and West Middlesex University Hospital (WMUH). This review will be looking at all the cardiology services the key providers offer to Richmond residents. This review should be able to discover if there is a mismatch in the population’s cardiology healthcare needs and the current resources they access.
Diagnostic pathway for suspected/known cardiology conditions
Case for change
Variation exists in the way patients within Richmond are investigated and diagnosed with a cardiology condition between GP surgeries. Furthermore, intra practice variation exists, as there are differences within a surgery on how each GP will manage a patient.
The decision by a GP to refer to cardiology can be multi-factorial. Many pathways require a referral to access an investigation or intervention which may only be provided in secondary care. Access to B-type natriuretic peptide (BNP) and an Echocardiogram (Echo) can influence the provider a GP will refer to. GPs may know the likely diagnosis of the patient but will need to conduct investigations to confirm this; a referral to the cardiology department could be the only route to certain investigations such as an Echo or 24hr ECG (a number of GP surgeries in Richmond do not have 24hr ECG monitors)[xli]. GPs may be influence by a number of factors to refer patients to a particular service, and this is not exclusively clinical terms. Factors that influence GP referrals highlighted by healthcare professionals and the GP survey include:
- Access to diagnostics
- Patient choice
- Proximity of provider to patients’ residence
- Relationship between clinical professionals
- Confidence in provider
- GP competence and confidence
- Lack of knowledge of services other local providers can offer
- Fear of long waiting lists for patients
In Richmond, it is currently unclear as to what diagnostic tests GPs have access to within their surgeries locally and where patients are referred to for any tests that cannot be conducted at the GP surgery. It is also unclear what the referral criteria are for GPs referring patients on for diagnostics, additional tests, rapid access clinics or direct access clinics. Furthermore, it is unclear what the patient pathways are or how many different pathways exist once a patient is identified with a suspected or newly diagnosed cardiology condition.
Since Richmond does not have its own hospital within its borough, a large majority of GPs do not have a choice but to refer patients to outpatient services in hospitals outside the borough for further investigation and treatment. The closest hospitals to the borough are Kingston Hospital (KHT), Queen Mary’s Hospital, Roehampton (QMR), St George’s Hospital (SGH) and West Middlesex University Hospital (WMUH), and in some cases ICHT (Hammersmith Hospital). Therefore patients from Richmond have access to variable diagnostics, clinical services and are referred under variable criteria. Another point to consider is that these hospitals also sit in different cardiac and stroke networks and may have differing protocols for different diagnoses.
Richmond also has community cardiology service based at Teddington Memorial Hospital (TMH). This service has been commissioned by Richmond CCG and is delivered by cardiologists from ICHT. This service was designed to be of benefit to Richmond patients by providing them access to a high quality standard of clinical cardiology services at a reduced tariff. However, not all GPs within the borough are unaware of this service, or are aware and do not refer their patients to this service, resulting in the service not being fully patronised by the residents it was designed for, and not reaching its financial benefit in terms of first outpatients appointment at a reduced cost rather than full tariff rate at hospital. Furthermore, the current community service is not comprehensive, as it does not have access to all the diagnostics necessary for cardiology, 5 days a week. If a number of services are not available or accessible 5 days a week, this could be a strong reason why a number of GPs do not refer to this service, resulting in lower than expected referral numbers.
Reason for reviewing cardiology:
- Cardiology had the second highest speciality outpatient appointment (OPA) spend in Richmond in 2012-13
- Unclear if is heart disease is being managed appropriately by the GPs/community
- CVD is one of the biggest causes of mortality in the UK and 1/3 (32%) of deaths in LBRuT are due to CVD.
- There is a 5 year gap in CVD mortality between the least and the most deprived wards in LBRuT.
- National publications such as commissioning guides from NICE on Cardiac Rehabilitation show that commissioning an evidence-based cardiology rehab service in the community has the potential to improve the quality of care of the patients and reduce in hospital admissions resulting in massive savings. Therefore , Cardiology has been included as a potential QIPP scheme for 2014/15
- The June 2013 Spending Round announced the creation of a £3.8 billion Integration Transformation Fund – now referred to as the Better Care Fund – described as ‘a single pooled budget for health and social care services to work more closely together in local areas, based on a plan agreed between the NHS and local authorities The Better Care Fund (BCF) offers a real opportunity to address immediate pressures on services and lay foundations for a much more integrated system of health and care delivered at scale and pace. The BCF is not new or additional money and commissioners have to make important decisions about how the grant is used. Cardiology service review offers an opportunity to explore potential areas for improvement and investment to save public spending in the future and improve quality of life, better care within the community and outside hospital.
Reviewing the cardiology outpatient activity and diagnostic tests will provide a better insight as to where GPs are referring to, what diagnostics are available at each site, and what each provider charges for various appointments, and identify any potential savings that can be made via changing patient flow to services or renegotiating provider services.
Case finding and risk stratification
Case finding
If a patient presents to the GP, is assessed and it is determined that the individuals QRISK is higher than 20%, and has hypertension or/and diabetes, then the individual is at risk of having coronary artery disease (CAD). For this category of patients, they should be monitored annually in primary care and asked clear questions about any chest pains or related symptoms.
Every practice should have a systematically developed and maintained practice-based register of people with clinical evidence of CHD, occlusive vascular disease and people with a CHD risk of >20% over ten years in place and actively used to provide structured care to those at high risk of CHD[xlii]
NICE recommends that people aged 40–74 years who may be at high risk of CVD should be identified in primary care by estimating their CVD risk from existing medical record data. These people should be prioritised in descending order of risk and offered a formal risk assessment if their estimated10-year CVD risk is 20% or more[xliii].
NHS Health Checks
In LBRuT, the national CVD risk assessment and management programme is part of the NHS Health Checks programme which was initiated in the community in 2009. Currently, it is being delivered to all LBRuT residents between 40 to 74 years of age who do not have any known CVD conditions. Other exclusions are also applicable. The programme is being delivered by 29 general practices, 7 pharmacies and a community outreach provider. The programme has been commissioned by the LBRuT which is a mandated service. LBRuT has adopted a targeted approach to tackle CVD related inequalities. These include targeting the most deprived areas of the borough and prioritising people with high risk CVD, severe mental illness, people with learning difficulties and carers. Research has shown that, these vulnerable groups are more prone to CVD as compared to the general population.
The programme has been a success story in LBRuT, as it has helped to identify more than 500 people with CVD and referred more than 500 people to various life style services. Since 2009, nearly half of the eligible population has been invited and approximately one-third have received a health check. Those with a high and medium risk are being proactively managed in the general practice. LBRuT’s success story has been acknowledged widely and has been shared nationally at various conferences and events.
Figure 10 Identifying people for full formal CVD risk assessment
Source: NICE Lipid modification (2010)
Figure 10 below gives a breakdown of the gender makeup of low, medium and high risk patients attending a health check between April and December 2013. Of the 3298 health checks completed between April and December 2013 59% of patients were female and 41% were male. This demonstrates that more females than males are accessing the service. In total there were 187 high risk patients identified within this time period; 151 of them were male, making up 81% of high risk patients. However, 65% of the low risk patients were female,
Figure 11 Risk level found in health checks by gender percentage between April and December 2013
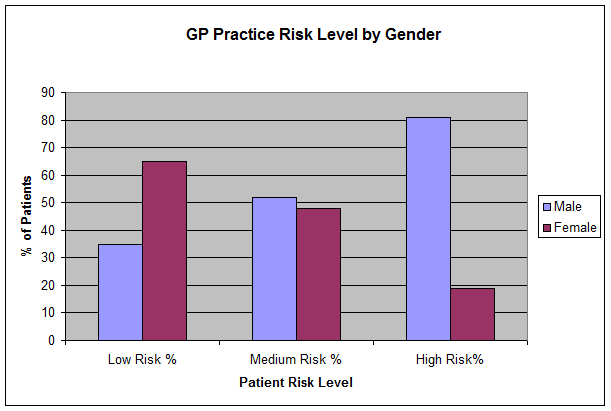
Source: Richmond NHS Health Checks Service Review 2013 (Draft)
The health checks data for Richmond demonstrate that male patients are more likely to be at a higher risk of getting the specific non-communicable diseases including CVD and hypertension than women.
Figure 12 Number of NHS health checks offered and completed by GP practice, 2012/13
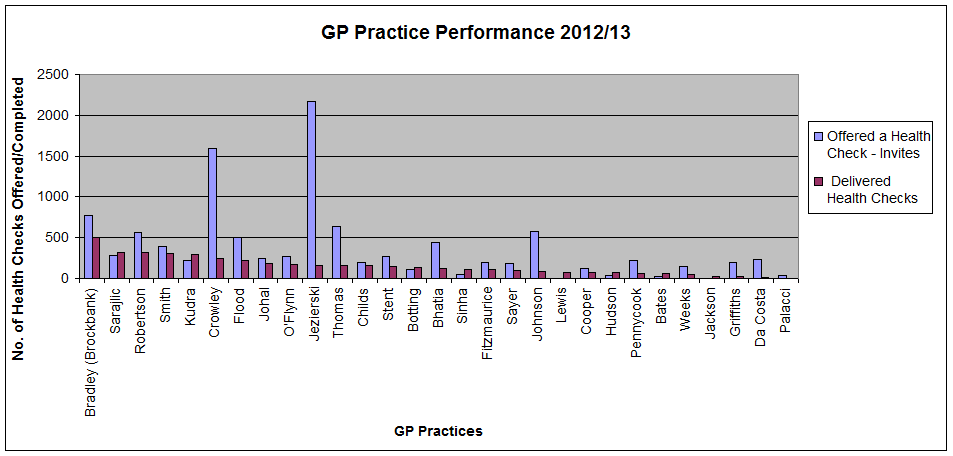
Source: Richmond NHS Health Checks Service Review 2013 (Draft)
N.B.: this graph has not been standardised by GP list size
Figure12 below demonstrates that out of the 19 boroughs analysed for the NHS Health Checks, Richmond completed the fourth highest percentage of health checks relative to its eligible population in the first two quarters of 2013/14 (6.1%). Richmond was also fourth best for the percentage of health check invites.
Figure 13 Comparison of performance by percentage of invites (invites divided by eligible cohort) and completed health checks (checks divided by eligible cohort) in the first two quarters of 2013/14 (April – October 13)
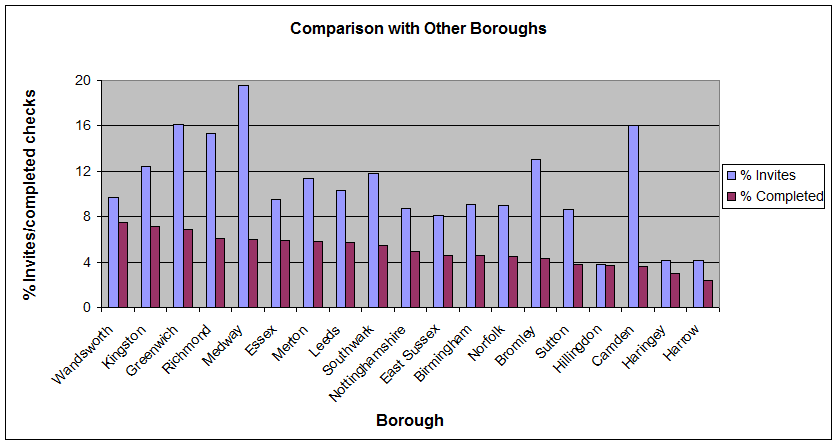
Source: Draft NHS Health Checks Service Review
For angina, diagnosis is usually based on the history of the patient[xliv]. The Rose angina questionnaire has been found useful to identify a number of angina patients; however this does vary in its sensitivity when compared with clinical diagnosis[xlv].
Patients with mental health conditions
A UK qualitative study demonstrated various barriers that may exist when trying to screen people with severe mental illnesses (SMI) for heart disease risk factors and/or interventions for primary prevention. These barriers include[xlvi]:
- Lack of appropriate resources in existing services
- Anticipation of low uptake rates by patients with SMI
- Perceived difficulty in making lifestyle changes amongst people with SMI
- Patients dislike having blood tests
- Lack of funding for CHD screening services or it not being seen as a priority by Trust management
It is necessary to be aware of these potential barriers and establish close links with the mental health teams on how to identify, treat and manage these patients. It has already been identified earlier in the review that over 20% of patient with heart disease suffer from depression/anxiety; meaning over 1/5 of people with heart disease in Richmond have a mental health condition, which equally needs to be addressed and managed in conjunction with heart disease.
Risk stratification
Risk stratification using clinical scores should be conducted to identify those patients with an ACS who are most likely to benefit from early therapeutic intervention[xlvii].
Local risk stratification conducted by the Public Health Intelligence team (PHIT) at Richmond can also be used to identify patients that have a number of morbidities and that may be at risk of having a cardiology condition, and should therefore be monitored by the GP.
Whilst the review team are aware of the contribution smoking makes to the risk and prevalence of CHD, the scope of this review does not include smoking cessation. More information on smoking cessation services and support in Richmon can be found on the Live Well Richmond website: https://www.live-well.org.uk/richmond/
Local Services
Cardiac and Stroke Network
In 2010, the Commissioning Support for London’s model of care for cardiovascular services[xlviii] recommended that cardiac and stroke networks should be implemented across England to consolidate treatment for these services, giving patients access to the best, specialised care to provide the greatest chance of survival. In London, five Cardiac and Stroke Networks were formed and Richmond sits within the catchment area for the South London Stroke and Cardiac Network (SLCSN). Each network has nominated stroke and cardiac tertiary centres whereby certain specialist cardiac and cardiothoracic procedures are only performed at these centres. St George’s Hospital is the tertiary stroke and cardiac centre primarily serving the south west London population. From 1 April 2013 the SLCSN work programme transitioned to the London Strategic Clinical Networks (SCN) hosted by NHS England.
Due to the geographic location of the network, there is more than one London Cardiac centre that is relatively accessible to Richmond residents. The other stroke and cardiac centres in London that a proportion of Richmond patients are regularly referred to by GPs or other providers are:
- Imperial College Healthcare Trust (ICHT) (Hammersmith, Charring Cross and St Mary’s Hospital)
- Royal Brompton and Harefield NHS Trust (RBH)
Specialised cardiology and cardiac service activity is concentrated in relatively few specialist centres to ensure a sufficient volume of activity is undertaken to develop and maintain expertise
The list below encompasses seven specialised service areas that specialist centres manage:
- Heart, lung and heart & lung transplantation services (including implantable ventricular assist devices) – There are seven nationally designated centres for adults and two for children in England.
- cardiac electrophysiology services
- inherited heart disorder services
- congenital heart disease services
- cardiac surgery and invasive cardiology
- pulmonary hypertension services
- cardiovascular magnetic resonance services
Governance
Governance is an important area within any type of service being provided to the community, especially healthcare. For Richmond patients, wide variation exists between the different cardiology services that are accessed by Richmond patients. This variation exists for a number of reasons:
- LBRuT does not have an Acute hospital within the borough
- Different London CCGs commissioning a variation of services
- GPs within the borough are not using a universal assessment and referral criteria for cardiology
The variation in services and governance has resulted in a number of LBRuT residents experiencing inequitable cardiology services, which can have an impact on their recovery time, and experience. It is the duty of LBRuT and the Richmond Clinical Commissioning Group (Richmond CCG) to ensure that LBRuT patients have access to the best service possible and are not discriminated against in the process of accessing these services. Similarly, Richmond CCG may not be commissioning appropriate services fit for the purpose and according to the local needs of the population.
General Practitioners (GPs) in Richmond
Once a patient is seen in clinic, the GP will decide if they require further testing. Dependent on the resources the GP has, they may be able to perform some tests, also known as ‘working up’ the patient before referring them on to the community services or outpatient service to have further tests and/or a cardiology appointment.
The GPs in Richmond do not have a universally agreed criterion for the referral of cardiology patients for further investigation. This inevitably means that cardiology/suspected cardiology patients that have GPs within Richmond have an inequitable service from the beginning of the pathway, as referral criteria differs from surgery to surgery, from GP to GP and amongst different cardiology outpatient services.
GP Cardiology Services and Provision in Richmond Questionnaire (LPIS) 2013
In November 2013, a cardiology service questionnaire was sent out to all the GP surgeries in the LBRuT. There was a 100% response rate, making the data collated reliable and demonstrable of what is happening in the community with regards to cardiology. However, a point to note is that the questionnaire was not completed by each GP, rather a GP on behalf of each surgery.
Serviceable equipment at practices in Richmond
Figure 13 (below) shows that most GP surgeries within Richmond possess an ECG and 24hr BP monitor. Therefore GPs should be able to perform these tests on patients instead of referring them to other services that will charge for these diagnostics. Only 2 practices in Richmond reported that they had an anticoagulation monitor. Anticoagulation monitoring necessary to ensure the anticoagulant blood levels are within the International Normalised Ratio (INR). NICE recommends anticoagulation monitoring for AF patients before and after cardioversion[xlix] (AF diagnosis, treatment and management in primary care to be covered in part 2 of the cardiology review).
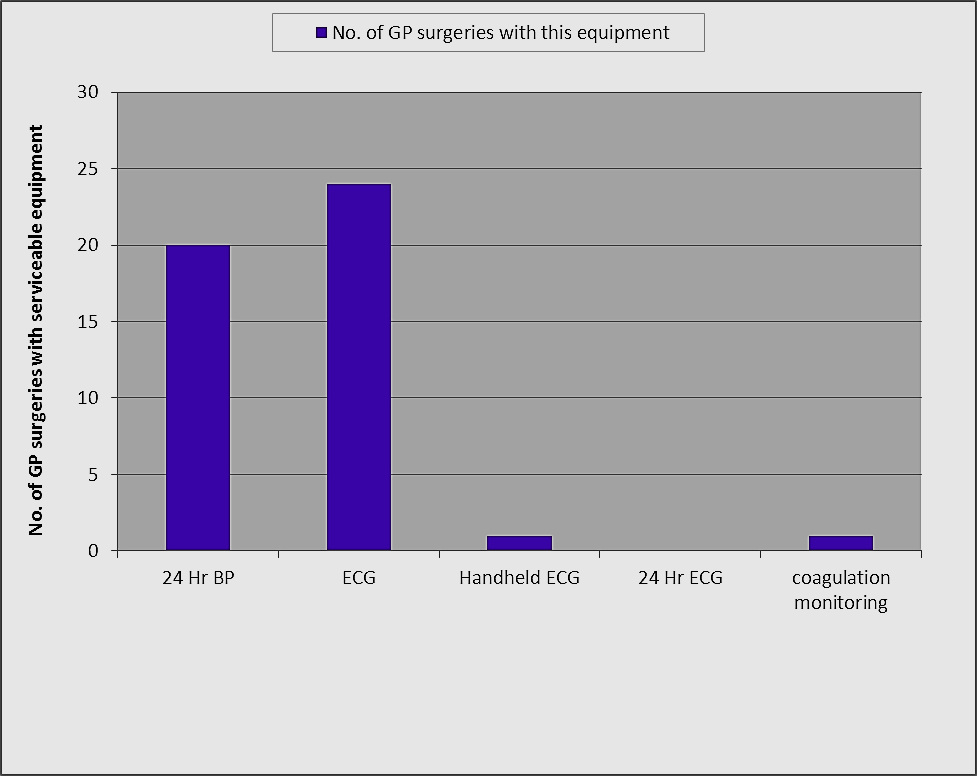
Figure 14 GP surgeries in Richmond with serviceable equipment
Source: Cardiology Services and Provision in Richmond Questionnaire (LPIS) 2013.
GP referral preference
Figure 14 (below) shows that the 22 out of 31 GP surgeries in LBRuT refer their cardiology patients to Kingston Hospital for further investigation or treatment. However, this does not imply that 22 GPs exclusively refer all their cardiology patients to Kingston cardiology services. 2/3 of LBRuT GP surgeries send cardiology referrals to KHT. The results also show that the community cardiology service is used by almost 50% of the GPs, shortly followed by QMR and WMUH. It was expected that the specialist (also known as tertiary) cardiac centres would not have a high volume of initial referrals, as they should not usually be the first point of call; however, a 5 GP practices stated that they refer some of their patients to ICHT for their first cardiology appointment. GPs response to the survey in regards to where they send initial referrals are not directly reflected in the overall activity and spend for the initial referral to key outpatient cardiology services.
Some GPs mentioned they were not aware of the Richmond community cardiology service at TMH, and would consider referring to this service in the future. Other GPs expressed their discontentment with their patients having to go to Charring Cross/Hammersmith/St Mary’s hospital for further investigations/secondary care once being seen at QMR or TMH because of the distance patients would have to travel. This indicates that the cardiology consultants from ICHT delivering community cardiology services at these sites refer patients that need further treatment to their base hospitals (CHX/HH/SMH), which is not always the closest specialist cardiac centre to Richmond residents. However, it may be the closest option for those living in the Barnes and East sheen area. Secondly, some of the tests or treatments carried out at ICHT could be carried out at other key providers that may be closer to the residents.
Figure 15 Preferred place of referral for outpatient appointments
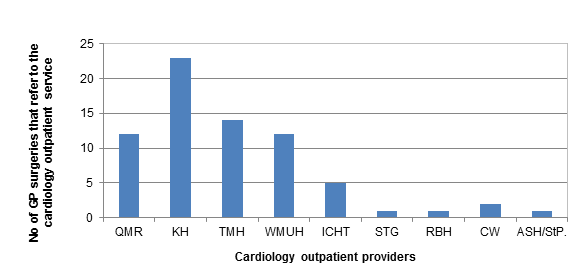
Source: Cardiology Services and Provision in Richmond Questionnaire (LPIS) 2013.
Types of clinics GPs refer to and ‘work-up’ tests
- Some GPs would not do any work-up at all – they would refer patient straight to clinic for this.
- Doing work up depended on the specific cardiology condition the GP suspected
- Dependent on GP access to services and what equipment they had in the surgery to carry out any tests.
- RACPC commonly referred to if patient expressed chest pain
- Unsure if patients referred to rapid access clinic are being referred appropriately.
How GPs manage post-cardiac event patients
- “Follow guidelines. Optimise blood pressure and lipids (but often lipid targets in hospital exceed outcomes achievable with community pharmacy advice
GPs opinion on what secondary care services could do to assist in the better management of cardiology patients
- “Improved access to diagnostics”
- “Clear, accurate and more informative discharge letters, specifying diagnosis and medication (s) prescribed”
- “Better education of patients’ before discharge”
- “GPs and secondary care clinicians to work together to redesign cardiology referral pathways”
- “Improve pathway for AF when diagnosed in A&E”
Overview about the service by GPs
- Need more communication between consultant and GP
- Would be useful to have easier access to ambulatory monitoring, which at present requires a referral to TMH cardiology clinic and likely classed as a new referral.
- QMR – onward investigation at SMH (ICHT) is too far for patients to travel
- Patients who go to QMR to be offered choice of hospital for onward referral according to the original agreement, all are referred on to SHM (ICHT)
Service improvement suggestions
- Look at risk calculators vs coronary calcium scores for those who are neither very high risk primary prevention (e.g. diabetes) no very low risk.
- Suggestion of GP Led Cardiology Clinic in the area (GPwSI)
- Providing an urgent email/telephone service would be a great improvement and beneficial to both GPs and patients.
- Community heart failure (HF) Nurse Specialist
- Would be useful to have easier access to ambulatory monitoring, which at present requires a referral to TMH cardiology clinic and likely classed as a new referral.
- New anticoagulants for cardiology or haematology
- Possibly arranging teaching sessions for GPs
The survey results have shown that Richmond GPs could do more in primary care to improve the level of care for cardiology, in terms of assessments and diagnostics carried out at primary care presentation. They also need to be better informed about the Richmond community services available, the SLCSN cardiac network provider and have access to the necessary equipment to be able to provide initial work up such as ECGs that are necessary for initial diagnosis. Over 57% of GPs have ECG and 24hr BP monitors, and should therefore be able to conduct the necessary initial work up necessary for suspected and known cardiology patients instead of these tests being done by providers and the CCG being charged for this.
The GP survey also highlighted the issue of patient choice (or lack thereof) at the point of onward referral from QMR and TMH to ICHT. All patients seen at these hospitals requiring further investigations or treatments are routinely referred to ICHT and are not offered the choice of going to other providers unless they state they would like to.
Community Cardiology services
Community services are designed to support primary care management of cardiac and suspected cardiac conditions through the provision of direct access diagnostic services and a community based one stop model of outpatient services. In this setting a patient can have all the necessary diagnostic testing done, then have clinic review. Dependent on the review, the clinician will formulate a management plan and send to the referring GP, or refer the patient to a cardiology outpatient department for further investigation and review with a cardiologist.
Community cardiology services should be able to carry out all the main diagnostics that GPs may not be able to in order to better determine the appropriateness of referring patients to secondary care. The service should act as a “gate-keeper” accessing outpatient cardiology services, however, this does not appear to be the case with the current ICHT commissioned community cardiology service based at Teddington Memorial Hospital.
Teddington Memorial Hospital (TMH)
For Richmond, TMH is the community hospital based within the borough. Queen Mary’s Hospital, Roehampton (QMR) is also a community hospital in the neighbouring borough with cardiology clinics being provided by ICHT cardiologists; however, it appears that Richmond patients are being treated at this service under the acute tariff and not community tariff as is being done at TMH.
In 2010, NHS Richmond and Twickenham (now Richmond CCG) signed a Service Level Agreement (SLA) with Imperial College Hospital Trust (ICHT) to provide community-based cardiology services outside of an acute setting for only NHS Richmond patients at Teddington Memorial Hospital (TMH). This service was designed to give easy access to Richmond Borough patients living in the Twickenham, Teddington and Hampton locality to local cardiology services. The aim of the community service is to reduce the amount of inappropriate referrals to cardiology outpatient departments in secondary care. It is also designed to give patients the benefit of local access to cardiology services- however; it does not provide a comprehensive cardiology service 5 days a week. This service does not have a rapid access chest pain clinic (RACPC) service, pain nurses, variation of diagnostics needed, and neither all-day diagnostics. The service also faces IT challenges which has an impact on sending patient diagnostics to other trusts.
The provision of blood tests and chest x-rays has not been included in the service delivery scope. Therefore, these tests should be completed by GP’s prior to patient’s attending appointment, or they have the option of referring patients to diagnostic facilities managed by Hounslow and Richmond Community Healthcare (HRCH).
TMH also hosts speciality cardiology clinics run by ICHT consultants:
- Arrhythmia clinics
- Hypertension
- Ischaemic Heart Disease (IHD)/ valve disorders
- Chest pain service (this is not a RACPC)
Table 4 Suspected conditions and the tests that would be performed at TMH
|
Conditions |
Diagnostic tests required |
|
Palpitation |
24hr ECG monitoring Echocardiogram (if indicated) ECG Bloods requested by GP prior to referral : thyroid function test, U&E’s, FBC |
|
Shortness of breath/Heart Failure
|
Echocardiogram ECG Bloods requested by GP prior to referral : U&E’s/ FBC/ Creatinin Chest X-ray requested by GP prior to referral |
|
Chest Pain
|
Exercise tolerance test (if indicated) Echocardiogram (if indicated) ECG |
|
Hypertension |
Echocardiogram (if indicated) ECG 24hr Blood Pressure Monitoring (if indicated) |
|
Murmurs |
Echocardiogram ECG |
Source: Imperial College Healthcare NHS Trust Service Level Agreement document for the Richmond Community Cardiology service (2010)
The community cardiology service provides one-stop direct access clinics for NHS Richmond patients referred by their GP. This service has access to the following diagnostics:
- 24hr ECG tests
- Echocardiogram
- Exercise tolerance test ( ETT)
The algorithm below describes what a typical patient journey from GP presentation to referral to the TMH community service and possibly beyond should look like in accordance with the SLA.
Figure 16 Step-by-step diagram flow of the patient pathway from GP presentation to TMH cardiology community service.
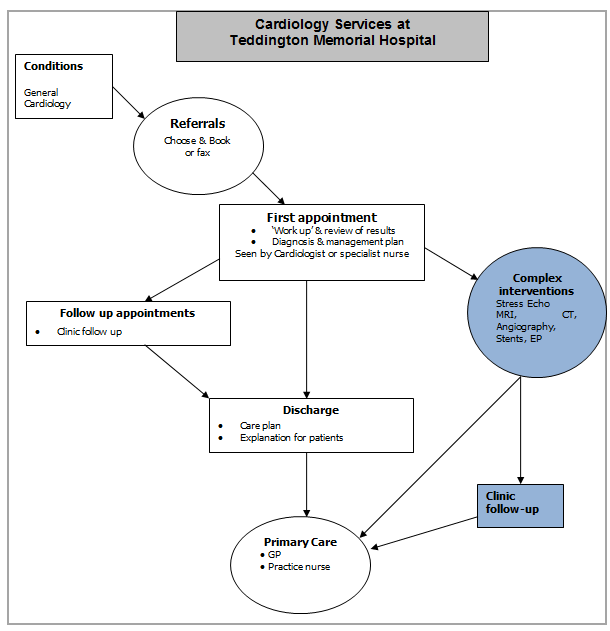
Source: NHS Richmond & Imperial College Healthcare NHS Trust, 2012.
N.B.: Symbols shaded in green signify activity in secondary care. The complex interventions mentioned on the diagram are conducted at ICHT, not at the community service. Also, the current SLA for the community service does not include a follow-up service; so this would also be done at ICHT before discharge back to the GP.
From the GP cardiology questionnaire it is apparent that not all GPs are aware of this community service commissioned especially for the Richmond community. Aside from that, a number of GPs are under the impression that QMR has been commissioned to provide a cardiology community service for LBRuT residents, and refer patients their as an alternative community service for Richmond; however this is not the case. Richmond patients referred to QMR are not being charged a community rate in the same way as the TMH service.
It is very important to know the number of patients seen at TMH that have onward referrals to providers far away from the borough, as the community service was established to provide a more convenient and accessible service for local residents. Therefore, sending them further outwards for secondary care whist there may be providers nearer by that can provide the same level of service does not appear to be the best choice for the residents. If the patient requires an onward referral to secondary care, there is not an agreed nominated provider that the community service should refer to as per the SLA; however, it appears that all onward referrals are sent to the same cardiologist that sees them at TMH at ICHT.
Challenges facing the community cardiology service in TMH:
- Low capacity attendance – not as many GPs are referring to this service as initially anticipated. The SLA stated that the maximum projected demand for this service was 6650, with the provider capacity able to service 4000 people. In 2012/13, the reported total activity for TMH was 1,232 appointments (of which 634 were direct access Echo appointments)[l]. This is less than half of the original projected activity (as per the SLA) for Richmond cardiology community service.
- 80% of referrals for direct access to diagnostics and appointments are booked by fax and not choose and book (C&B); however, TMH clinics are available via C&B. This means that a high number of referrals do not pass through RCAS for review of appropriateness.
- Use of the word community and the effect it has of patient perception.
- Lack of adequate space currently hired to have a fully functioning cardiology service
- IT- the IT system in TMH is not connected to ICHT, or any of the other key providers IT systems, causing some initial delay in receiving the test results. This is likely to result in tests being repeated and incur duplicate costs to the CCG for the same test.
- Service prices are due to increase in the financial year 2015/16 (the current contract has been rolled over for financial year 2014/15 with no financial changes to current agreed costs). With ICHT due to increase the charges for the community services, it is time to evaluate the current service to see if it is meeting the patient’s clinical needs and delivering to expectations.
- Lack of all the diagnostics and expertise needed to have a comprehensive community cardiology service to adequately ‘triage’ patients and refer them onwards to a provider or back to the GP as appropriate.
Queen Mary’s Hospital, Roehampton (QMR):
QMR has GP direct access clinics for cardiology patients as well as new patient assessment clinics and some rapid diagnostic clinics. QMH is a part of St George’s Healthcare NHS Trust and is within the Wandsworth borough; however, a proportion of Richmond GPs refer Richmond patients to this service. Even though QMR cardiology outpatient services are accessible for Richmond patients, it sits in a different borough with a different provider. Furthermore there is a lack of clarity about what QMR about the community service provision for Richmond patients i.e. if their services are being charged at a lower community tariff or at the normal acute provider tariff. Therefore it is necessary to understand what type of service is hosted by QMR, the activity of Richmond patients attending this service and the financial implications. If a high proportion of Richmond cardiology residents are having outpatient appointments at QMR, it would be reasonable to explore the possibility of setting up a community service agreement similar to the service delivered at TMH.
Prior to this review it was thought that the QMR cardiology service is part of Richmond’s community service. However, through this review it has been discovered that QMR has not been commissioned by Richmond CCG to deliver community cardiology services to Richmond patients. This means that any services procured at QMR will be charged at a tariff that may well be higher than the present community tariff at TMH.
There is only one cardiology service operating at QMR, which is provided by ICHT. This service has not been negotiated by Wandsworth CCG in the same manner in which Richmond CCG has done with ICHT for the community service at TMH.
Aside from the general cardiology outpatient’s clinic, QMR hosts other cardiology clinics:
- Specialised arrhythmia clinics (run by a ICHT electrophysiologist consultant and CNS)
- RACPC (see appendix 10 for pathway)
- Rapid access diagnostic murmur clinic
- Rapid access diagnostic heart failure clinic
- Rapid access diagnostic Hypertension clinic
N.B. The rapid access cardiology clinics provide a range of same day diagnostic tests which appeals to a number of Richmond GPs.
QMR service has access to the following diagnostics for cardiology:
- ECHO
- Pacemakers
- ECGs
- ECG holter monitors
- BP monitors
- Patient Activated Recorders
- Full Lung Function Service including reversibility studies
Patients initially seen at QMR cardiology outpatients department will be reviewed by an ICHT consultant. If they feel further diagnostic evaluation is needed that is not available at QMR, or treatment is required, then these patients are routinely referred directly to St Mary’s Hospital (ICHT). QMR’s invasive cardiology service is provided in full by ICHT. At present, patients are not referred to SGH or any other hospital unless they express their opinion to go elsewhere.
Richmond Clinical Assessment Service (RCAS):
Richmond has commissioned a peer review system which provides triage of eligible referrals from GPs to acute care. Experienced local GPs review routine GP referrals and help to decide the best option for assessment and treatment, providing peer support. Patients referred to rapid access clinics or urgent out-patient appointments do not have their referrals reviewed by RCAS.
The service was developed with the aim of providing NHS Richmond patients with equitable access to appropriate services. NHS Richmond commissioned this service based on the local needs assessment and analysis that identified high referral rates from primary to acute care. RCAS service uses the telephony and booking service more commonly known as ‘Choose and Book’ (C&B) to gain access, review and manage referrals from Richmond GPs to acute care, The assessors use the South West London Effective Commissioning Initiative
(SWL ECI) policy and local guidelines as a triage tool and if further evidence is required this is discussed with LBRuT Public Health team.
Figure 17 Number of cardiology initial GP referrals to key providers by GP practice over a 9 month period from March to November 2013
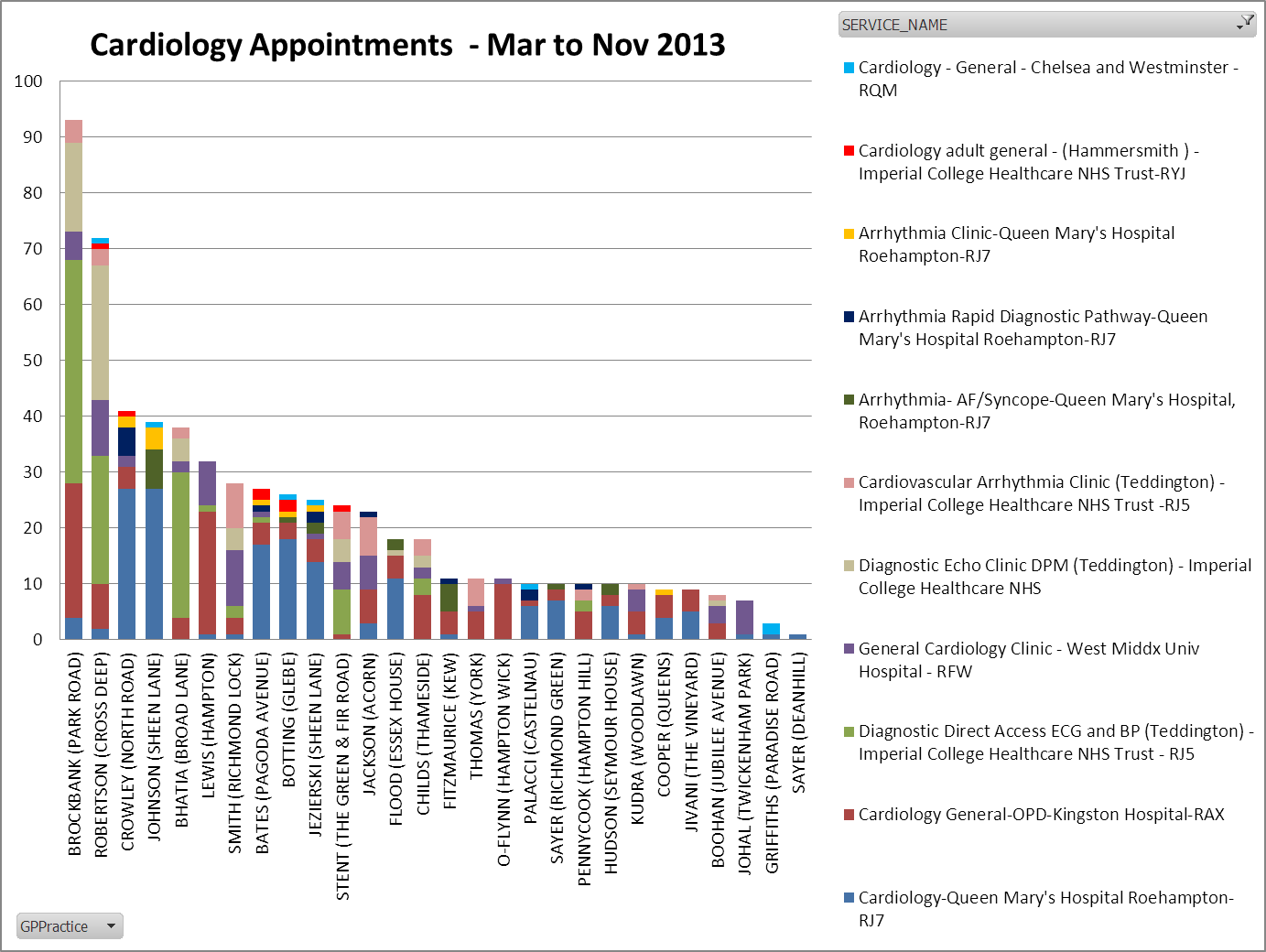
Source: RCAS
It is important to note that approximately 50% of GPs use the RCAS service for routine referrals and approximately 50% of all cardiology referrals are made through RCAS. There are a notable proportion of GP referrals being made via fax and consultant letters. This demonstrates the various pathways that exist to access cardiology services in an outpatient setting,
This graph has highlighted the following:
- There are various outpatient services relating to cardiology that GPs can refer to.
- The GPs refer most to KH, TMH and QMR. This confirms the findings in the GP survey, with 2/3 of practices referring to Kingston. However, this graph is able to show the proportion of referrals sent to different providers, giving us further indication of GP preference.
- Park road surgery has the highest number of referrals during this period at 94; this is over 20 more referrals than any other surgery within the same timeframe. The majority of referrals made at this surgery are primarily to TMH cardiology and direct access Echo service, then KHT. This surgery sits within the Teddington and Hampton clinical network area and is in close proximity to TMH.
- 11 GP practices in Richmond use QMR as their first preference for cardiology outpatient services.
- 11 GP practices refer their patients to the TMH arrhythmia clinic, whilst 6 different GPs refer their patients to the QMR arrhythmia clinic, albeit smaller referral numbers.
- 12 GP practices refer cardiology patients to WMUH, albeit at varying preference. Only two GP practices use WMUH as their first preference for cardiology referrals.
- 2 GP practices refer directly to Chelsea & Westminster Hospital (C&W) and 5 GP surgeries refer directly to ICHT (Hammersmith Hospital). These results corroborates the GP survey response, showing few GPs referring directly to ICHT, therefore, they should not record a high number of first attendances.
- This graph shows that none of the GPs in Richmond refers their cardiology patients to SGH via RCAS in the first instance.
Rapid access chest pain clinics (RACPC) and direct access clinics
In 2000, the National Service Framework for coronary heart disease identified rapid access chest pain clinics (RACPC) as the appropriate model of choice for the assessment of patients presenting with suspected angina, with chest pain as the primary characteristic.
Patients that present to the GP with chest pain should be referred to the RACPC for specialist assessment. The RACPC clinics are designed to provide a one-stop service involving clinical assessment and investigations to confirm or exclude angina coronary artery disease (CAD). The clinics also set the patients onwards to evidence-based treatment (revascularisation).
There is a lack of knowledge around what is happening across the borough in regards to RACPCs. Services need to be mapped to understand if things are working well, or if there is a need to commission something different.
Direct access clinics are usually walk-in or appointment services for diagnostic tests. These clinics do not include an assessment or consultation with a clinician.
Current Service Providers
Richmond GPs currently refer patients to Rapid Access Chest Pain Clinics (RACPC) at the following providers:
- Kingston Hospital NHST Trust (KHT)
- West Middlesex University Hospital NHST Trust (WMUH)
- St. George’s Hospital (SHG)
- Imperial College Healthcare NHS Trust (ICHT) (Charing Cross, ST Mary’s and Hammersmith Hospital)
- Queen Mary Hospital, Roehampton (QMR)
- Royal Brompton and Harefield Healthcare NHST Trust (RBH)
Each RACPC has its own referral criteria usually contained within the general cardiology referral proforma, so the reasons/conditions for referral may differ – even if only slightly. An important point to highlight is that the Richmond community cardiology service at TMH does not have a RACPC. The result of this means that fewer patients are referred to this service, reducing the capacity seen and patients are referred to their closest RACPC service which is usually WMUH.
Kingston Hospital NHS Trust (KHT) rapid access clinic:
Kingston hospital runs a cardiology rapid access clinic 4 times a week.
West Middlesex University Hospital (WMUH) rapid access clinics:
The Rapid Access Chest Pain Clinic (RACPC) at WMUH conducts specialist assessment of patients with suspected new onset Angina within two weeks from referral. This service also identifies cardiac risk factors and enables people to assess their values and contemplate behaviour change.
St Georges Hospital rapid access clinic:
The Rapid Access Chest Pain Clinic (RACPC) at SGH is accessible 5 days a week and performs same day diagnostics.
Queen Mary’s Hospital, Roehampton (QMR) rapid access clinics:
QMR hosts rapid access clinics for chest pain, rapid arrhythmia, heart murmur and hear failure.
Imperial College Healthcare NHS Trust (ICHT) rapid access clinics:
RACPCs are available at Hammersmith, Charring Cross and St Mary’s Hospital five days a week.
Royal Brompton & Harefield NHS Trust (RBH) rapid access clinic:
RBH has RACPC’s two days a week; patients are seen by appointment only.
Hospital outpatient and diagnostic services
Kingston Hospital NHS Trust (KHT):
GPs are able to refer to KHT’s one-stop cardiology clinic via the ‘choose & book’ system, as well as faxing referrals to the rapid access and walk in diagnostic services.
Some specialist cardiology clinics at KHT are run some jointly with St George’s Hospital NHS Trust (SGH) clinicians, including interventional cardiology consultants and a consultant cardiac electrophysiologist. KHT offers a range of diagnostic tests, and has its own catheter laboratory to conduct invasive tests.
The following diagnostic tests are available:
- ECG and ambulatory/24 hour ECG
- BP
- Exercise Tolerance Test (ETT)
- ECHO
- Trans Oesophageal ECHO
- 7 day event recorders
- Diagnostic angiography
- Myocardial perfusion imaging
KHT has a dedicated cardiology in-patient ward with a ‘step down’ unit to manage rehabilitation of coronary patients. Cardiology procedures performed at KHT include permanent pacemaker insertion and cardioversion day case treatment.
The criteria for referring patients initially seen at KHT cardiology outpatients department to SGH are as follows:
- Patients who require percutaneous coronary intervention (PCI) and structural heart interventions,
- Complex pacing and cardiac electrophysiology (EP) procedures etc.
- Advanced imaging such as stress Echos or cardiac MRIs.
- Patients who require a specialist OP opinion such as Inherited Cardiac Conditions (ICC), Structural Heart Disease or pulmonary hypertension, and in some cases refractory hypertension.
- Patients who require cardiothoracic surgery.
There is a joint Service Level Agreement (SLA) between KHT and SGH to provide rapid access to specialist tertiary services locally for patients having their outpatient appointments of secondary care at KHT. This results in a number of inter-hospital transfers from KHT to SGH for specialist cardiac services in accordance with the pan-London cardiac services. Figure 17 (below) depicts the cardiology patient flow that exists between KHT and SGH.
Figure 18 Flow diagram to show the patient cardiology referral pathway flow between KHT and SGH
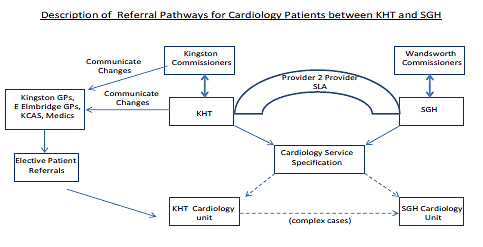
Source: Cardiology at Kingston Hospital (2012)
The criteria for referring admitted cardiology patients from KHT to SGH are as follows:
- Patients who require emergency coronary intervention (high risk NSTEACS), pacing or EP procedures.
- Patients who require urgent, rather than emergency procedures.
- Patients who require urgent cardiology/CT surgical MDT management (e.g. complex endocarditis)
- Patients who require inpatient cardiac surgery
There are no specific criteria for the referral of cardiology patients from KHT to RBH as the designated cardiac referral centre for KHT is SGH. However, when it is apparent that a timely transfer of an inpatient (IP) for further care is not possible, KHT liaise with other interventional centres for continued management, with RBH being close by and accessible. In other cases when the patient has had a long history of management by clinicians at the RBH or multiple previous procedures (i.e. well-established on a pathway there); it is deemed reasonable by KHT clinicians to re-refer the patient back there to ensure continuity of care.
Kingston CCG is also running a pilot Patient-Centred Angina self-Management programme (PCAM), which is due for review in April 2014. The intervention is a community based outpatient education programme with an initial 1:1 session followed by four group sessions and a follow up group session at 3 months and 12 months. There is some evidence that these types of self-management programmes can reduce health care utilisation such as hospital admissions. Patients selected for this programme will be either those with refractory angina[1] or those contemplating scheduled palliative Percutaneous Coronary Intervention (PCI)[2] with stents or balloons.
Richmond CCG decided to wait till the Kingston PCAM pilot’s evaluation and findings were made available. If appears that the Kingston CCG PCAM pilot is successful and shows an improvement in the patient’s quality of life (QoL) as well as demonstrating significant cost savings, then Richmond CCG will consider commissioning the service. However, it will be necessary to aligned with the existing services such as the Expert Patient Programme and cardiac rehabilitation programme with PCAM.
St George’s hospital NHS Trust (SGH):
The cardiac unit at SGH is a specialist tertiary referral centre for all types of adult cardiac and thoracic surgery and is the cardiac centre that primarily serves the south west London area.
SGH are currently in the process of expanding their cardiac department with the addition of 10 new catheter beds and a new treat and return unit in the first quarter of 2014. This should create more capacity for cardiology patients at SGH. Two pathway co-ordinators are also in the process of being appointed at SGH, with these roles being pivotal in the timely management of patient care and any necessary transfer of patients to and from SGH.
The following diagnostic tests are available at SGH:
- Direct access:
- ambulatory BP monitoring
- electrocardiography
- ambulatory and cardiomemo ECG monitoring
- ECG holter monitoring
- Cardiac MRI
- exercise tolerance testing (ETT)
- cardiac CT
SGH has an established adult congenital heart disease service and can perform a number of congenital interventions in the form of atrial septal defect and patent foramen ovale closure procedures.
West Middlesex University Hospital NHST Trust (WMUH):
WMUH provides an open access walk-in service for GP referred patients requiring routine ECGs with physiologists to provide initial ECG interpretation and referral to the relevant medical team. Where possible, WMUH provide same day diagnostic tests for all the cardiology clinics offering a one stop (direct access) service.
Below is a list of the cardiology diagnostics available at WMUH:
- 24 hour, 48 hour and extended direct access ECG holter monitoring
- Event recording
- 24hr BP monitoring
- Direct access exercise tolerance testing (ETT)
- Direct access simple/complex/agitated saline/contrast Echo’s
- Treadmill and dobutamine stress Echo
- Cardiac CT and calcium scoring
WMUH has a dedicated Cardiac Care Unit (CCU) for inpatients, however it does not have a catheter lab; therefore patients requiring this service are referred to other providers:
- ICHT for out-patient catheter services
- ICHT and RBH for in-patient catheter services
- RBH for complex heart failure catheter services
For patients that require invasive cardiac tests and cardiac/cardiothoracic interventions and other specialist cardiology services in secondary care, the majority would be referred to ICHT (HH); this is the cardiac centre in the North West London Stroke and Cardiac Network and is the closest cardiac centre to the hospital. WMUH also has a close relationship with RBHT and also refers a majority of its cardiothoracic patients to their service for further investigation and treatment. WMUH works with both ICHT and RBH on the non-elective pathway to offer patients a choice of provider and to minimise delays in the process of care.
The criteria for referring admitted cardiology patients from WMUH to ICHT are patients who require interventional treatment including:
- coronary artery bypass graft (CABG)
- Percutaneous coronary intervention (PCI)
- Complex electrophysiology (EP)
Referral from WMUH to RBH would occur for complex heart failure (HF) patients needing a full assessment including for cardiac transplantation
Imperial College Healthcare NHS Trust (ICH):
The cardiology services for this trust are spread across three hospital sites; Hammersmith Hospital (HH), St. Mary’s Hospital (SMH), and Charing Cross Hospital (CXH); each having their own outpatient appointments and diagnostic equipment. Patients are usually referred to these hospitals for further investigation and/or treatment by community – based cardiology services (TMH, QMR) or a district general hospital (WMUH). The trust also has a service whereby GPs and practice staff can contact their cardiology medical specialists directly with clinical queries and questions through the Trust’s new pilot GP advice service.
HH is one of the eight nominated heart attack centres in London, providing invasive tertiary cardiology and cardiothoracic services primarily for the North West London area. HH has specialist expertise in the emergency treatment of patients with acute coronary syndromes. The International Centre for Circulatory Health (ICCH) is based at SMH.
The pathway for Richmond patients that have their first cardiology outpatient appointment at WMUH and will require further investigation and/or treatment are referred to HH. Patients seen at QMR and TMH requiring further investigations and/or treatment are referred to SMH.
Private services
The LBRuT is one of the most affluent boroughs within London with over 50% of the population within the least deprived quintiles and less than 1% within the lowest deprivation quintile. With this type of population mix, it is noted amongst the local GPs that there are a proportion of patients that prefer to use the private care system for further investigations and treatment once they are told by their GP that they may have a suspected cardiology condition. However, it is not clear whether data relating to their condition once they are treated and discharged back to their GP is captured by the QOF programme.
Private diagnostic service
InHealth are a private diagnostic service provider, with direct GP referral, in addition to the Imperial community based service at TMH. The InHealth contract is managed by NHS England and had a 15% savings on tariffs; however this contract will terminate at the end at the end of March 2014. The imaging reports conducted by InHealth are sent back to the GP; however the GPs have expressed issues with the interpretation of the results and this seems to have adversely affected the number of referrals and led to underutilisation of the service by GPs.
The results from the LPIS Richmond GP survey (2013) as well as soft data demonstrate that none of the GP surgeries in Richmond actively refer their patients to InHealth for cardiology imaging diagnostic tests.
Activity and financial costs of current services
GP referrals to cardiology outpatient services have the second highest known speciality spend in Richmond in 2013, at 9% of overall spend (see figure 18). This indicates that there is high volume usage of cardiology services, and a high proportion of the population that require cardiology services within the borough, linking up with the earlier intelligence highlighting that a large proportion of the elderly population have a cardiology condition, as well as heart conditions being associated with other co-morbidities. This could also mean that there could be a proportion of referrals to cardiology outpatients by GPs for symptoms and conditions that could be better directed to a more suitable service or department (e.g. community services or conditions that that could and/or should otherwise be managed in primary care). It is also important to note how GP belief of the best services for their patients is an important factor that comes into to play when referring patients to cardiology services.
Figure 19 Clinical specialities in Richmond CCG with the highest referral costs for the first GP referral outpatient appointment (OPA).
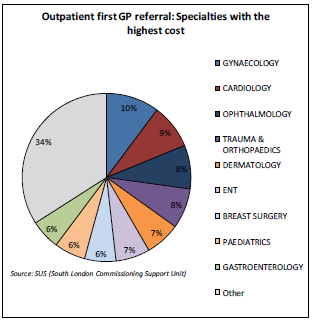
Source: Richmond CCG Clinical Network Data Pack (2013)
Referral activity
As mentioned earlier, Richmond GPs do not have a universal criterion for the referral of patients to cardiology services. Therefore destination of cardiology referrals will be distributed amongst service providers for a number of reasons including; proximity to referral centre, GP preference, access to timely diagnostics and speciality services. Richmond Public Health Intelligence (PHI) have utilised the activity data from SUS the reported activity by providers for cardiology services 2012/13(see table 6 below). The reported activity data provided by SUS is for Richmond CCG; therefore it does not include LBRuT residents that use GPs outside the borough. In the same circumstance, it does not include non-residents that use Richmond GPs.
Table 5 Richmond CCG Cardiology outpatient referral activity to key providers in 2012/13
|
Appointment type |
Activity |
Total activity |
||||
|
KHT |
ICHT |
RBH |
SGH (including QMR) |
WMUH |
||
|
First OPA referral |
598 |
1,680 |
71 |
1,655 |
481 |
4,485 |
|
Follow-up appointments |
673 |
998 |
1,172 |
805 |
460 |
4,108 |
|
Total number of appointments |
1,270 |
2,678 |
1,243 |
2,460 |
941 |
8,593 |
Source: Source: SL CSU, 2012/13
NB: QMR activity numbers are counted with SGH.
Key points to note from table 6:
- ICHT has the highest referral numbers of all Richmond key providers; however they are one of the least referred to for the first outpatient appointment. Due to the complexity of the way data is coded and collected, it is not possible to decipher whether the activity at the community cardiology service provided by ICHT at TMH is included in the reported activity for ICHT. If this is not the case and the ICHT activity does not include TMH, then it would appear that patients that are having follow-up appointments at ICHT as a result of their first appointments at TMH, QMR and WMUH and these appointments are being counted as first appointments instead of follow-ups, and are therefore being charged as such.
- A high level of follow-up activity has been identified at RBH. High follow-up activity has also been identified by other CCGs. RBH is a highly specialised centre; however, the transplant centre is based at Harefield hospital (which would require regular follow-up) and not Royal Brompton Hospital.
- QMR referrals and appointments are counted together with SGH, as QMR is part of the trust. From the GP survey and the RCAS referral data, it would be safe to assume that a large proportion of the referrals are from QMR. This assumption is verified further from the SL CSU, as no expenditure for patients’ first outpatient appointment are recorded for SGH (see table 8).
The SUS data was unable to differentiate the activity that occurred at ICHT and TMH, similarly with STG and QMR due to coding issues. Therefore, we have used the activity values provided by SL CSU to give us an indication of the outpatient activity that took place at TMH and QMR in 2012/13 (Table 7). Activity reported for TMH and QMR by SL CSU:
Table 6 Cardiology outpatient referral activity to TMH and QMR
|
Appointment type |
Activity |
Total activity |
|
|
TMH |
QMR |
||
|
First OPA referral |
1,040* |
1529** |
2,569 |
|
Follow-up appointments |
192 |
417 |
609 |
|
Total number of appointments |
1,232 |
|
3,178 |
Source: SL CSU, 2012/13
* 633 out of 1,040 appointments are for Echo’s that require booked appointments.
** 1,333 out of 1,529 appointments are for cardiology tests that require outpatient booked appointments.
The SL CSU report for QMR demonstrated that the total first outpatient appointment activity was 1,529 (including cardiology tests that require clinical appointments) which is approximately 90% of the activity reported by SUS for first outpatient appointments at SGH.
Trend in referral activity
Table 8 (below) shows an overall increasing trend in activity for first cardiology outpatient appointments in Richmond CCG from 2009/10-2012-13.
Table 7 Richmond CCG total activity for 1st cardiology outpatient appointments from 2009/10 to 2012/13
|
First cardiology appointments |
||||
|
Provider |
2009/10 |
2010/11 |
2011/12 |
2012/13 |
|
ICHT |
319 |
1,016 |
1,315 |
1,680 |
|
STG (incl. QMR) |
1,132 |
1,521 |
1,711 |
1,655 |
|
KH |
572 |
617 |
609 |
598 |
|
RBH |
104 |
76 |
86 |
71 |
|
WMUH |
692 |
615 |
475 |
481 |
|
Other providers |
141 |
138 |
126 |
110 |
|
SLA Agreed Total |
2,960 |
3,983 |
4,322 |
4,595 |
Source: SL CSU, 2014
Total referral numbers have gone up by approximately 1,600 appointments between 2009/10 and 2012/13.
Figure 20 Richmond CCG total activity for 1st outpatient cardiology appointments from 2009-10 to 2012-13.
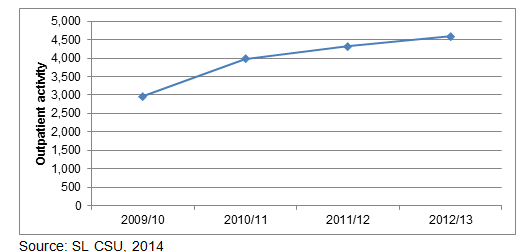
Since the commissioning of the community cardiology service in 2010, there has been a marked increase in the number of referrals for first outpatient appointments to ICHT cardiology department. In 2009/10 (pre- community cardiology service at TMH), the number of first appointments at ICHT were 319 (10% of the overall appointments in 2009/10). In 2012/13 (3 years post-community cardiology service), the number of first appointments at TMH were 1680 (37% of overall appointments in 2012/13). This shows over 500% increase in referrals to ICHT since 2009/10-2012/13. However, it is not clear from this data how many of the ICHT appointments actually taking place at the community cardiology service, as ICHT is the provider and the data services currently have not been able to differentiate the appointments in different locations. Nonetheless, this still demonstrates that the introduction of the Richmond community cardiology service provided by ICHT at TMH has had an impact on ICHT cardiology outpatient activity by significantly increasing activity. From the increase in activity for first appointments alone, it does not appear that the commissioning of the cardiology community service for the borough has supported the fulfilment of the Quality, Innovation, Productivity and Prevention (QIPP) agenda for Richmond over this period.
Figure 21 ICHT activity for 1st outpatient cardiology appointments from 2009-10 to 2012-13.
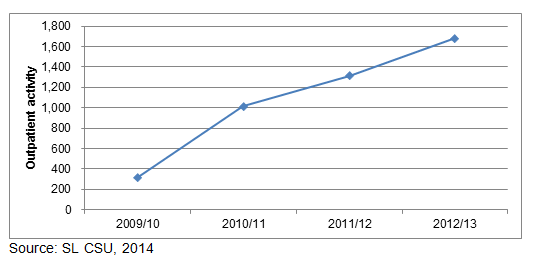
Figure 21 (below) shows the GP cardiology referral numbers by practice for 6 months in 2013, which most practices are referring within the Richmond average level. Hampton Hill practice shows it has over double the average amount of cardiology out-patient referrals over this period. The GP survey results show that Hampton Hill surgery refers patients to the ‘1-stop’ service mostly for diagnostics and that they are currently not utilising their ECG machine due to time factors and a lack of trained personnel. This surgery is in the Teddington area and a number of the appointments recorded could be because of the direct access to diagnostic services at TMH; however it is not known whether the number direct access appointments will be enough to mitigate the reason for a referral rate so high above the mean. However, the RCAS data for Hampton Hill shows that they have low cardiology referral numbers; this may indicate a preference with fax or written referrals for this surgery. TMH has also confirmed that a large number of their referrals are received by fax.
Figure 22 First GP referral to cardiology outpatient service by GP practise – age and sex standardised rate per 100,000 (April-October 2013)
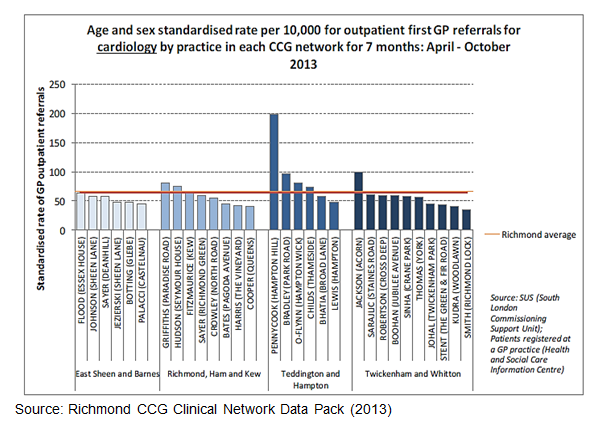
Source: Richmond CCG Clinical Network Data Pack (2013)
The cardiology review has been able to identify and highlight the current patient pathway for Richmond patients with our key providers (illustrated in figure 22 below). The curved arrows show the patient flow. The black arrows signify the first cardiology out-patient referral appointment from a community cardiology service. The red arrows signify the second patient referral from one secondary care hospital to another secondary care hospital. The diagram has demonstrated three different referral pathways by which patients final destination will be at ICHT. The diagram also shows the patient’s cardiology referral pathways and how the pathways can be delayed by attendance at providers that cannot offer all of the services they may require. It also shows that the CCG could be charged twice for patients attending two or more cardiology outpatient departments in one episode of care.
Figure 23 Cardiology referral patient flow for Richmond patients from GP to secondary care
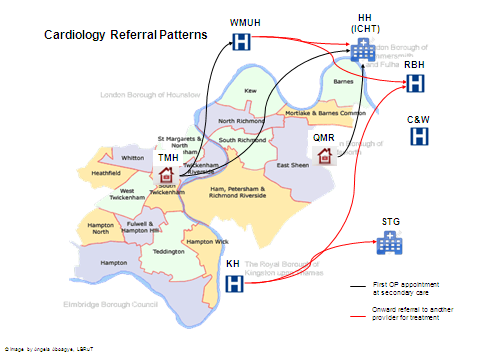
Costs
In 2012/13, the South London Commissioning Support Unit (SLCSU) reported that Richmond CCG spent approximately £3.7m on Cardiology services (in-patient and out-patient activity) for cardiology services provided by its main acute trust service providers. The total spend for in-patient services was £2.4m, and £1.3m for out-patient services.
The SL CSU oversees the payment to NHS providers from Richmond CCG for the services used by LBRuT patients. SLCSU receives the data from SUS which contains all the activity of attendances and procedures, the data is “cleaned’, activity is confirmed, adjustments are made in terms of any existing agreements and costs. Payments for services used are paid quarterly and a final payment is made at the end of the financial year which may include any discrepancies in activity, underpayment, etc.
For 2013/13 national tariff cost for a Cardiology first OPA with a single professional is £166, with multi-professionals £192. The national tariff for a Cardiology follow-up OPA with a single professional is £93, with multi-professionals £133.Each Trust adds their MFF to the national tariff to derive the total price charged. However, Richmond CCG has a local price for TMH first OPA which is less than the national tariff.
Table 8 Summary of overall cardiology spend with key providers (including in- and out-patient services)
|
Provider |
Cardiology spend (£) |
||||
|
First OPA |
Follow-up OPA |
Total Outpatient |
Total Inpatient |
Total |
|
|
KHT |
148,899 |
81,522 |
230,528 |
320,919 |
551,446 |
|
ICHT |
139,394 |
68,754 |
402,470 |
822,785 |
1,225,225 |
|
QMR |
101,043 |
53,201 |
232,000 |
– |
232,000 |
|
RBH |
21,850 |
122,988 |
188,683 |
509,536 |
786,507 |
|
SGH |
|
96,831 |
97,761 |
595, 559 |
692,390 |
|
TMH |
76,047* |
17,228 |
144,288 |
– |
144,288 |
|
WMUH |
83,976 |
55,928 |
151,137 |
163,409 |
314,546 |
Source: South London Commissioning support unit (SLCSU) (2013),
* An additional £50,919 was also coded as spent for the OP first appointment for an ECHO, which would bring the cost for first OPA at TMH to £126,966.
Findings from table 9:
- It is necessary to recognise that the first and follow-up appointment columns do not automatically equal the overall outpatient expenditure; the figures can be challenging to breakdown into exact cost items. This has been explored with SL CSU.
- Over one third of Richmond CCG overall spend on cardiology outpatient services is with ICHT. The trust outpatient services came to a total of £402,470. If this value is added to the total spend of the ICHT community cardiology service at TMH, this will come up to approximately £550,000.
- At TMH, the total expenditure came up to just under £150,000 (approximately £50,000 was solely for direct access Echo’s). If this amount is added to the ICHT expenditure, the total amount Richmond CCG has spent with ICHT.
- The total of first and follow up appointments at ICHT comes up to £208,148. However, the total outpatient activity costs amount to £402,470. This means that approximately £200,000 is being spent in outpatient services at ICHT, separate from outpatient first and follow-up appointments.
- There is a high inpatient spend for Richmond patients at ICHT. This could be due to the fact that it is a tertiary centre that deals with special complex cases that will take more to treat.
- There were no reported or paid costs for first appointments at SGH. This indicates that the majority of first appointment referral activity stated earlier for SGH was for QMR. However, it could indicate a coding issue with the provider and data utilised by SL CSU. The issue of no reported costs for first outpatient appointments has been raised with SLCSU, but are yet to receive a response from them as to the reason why.
- There is around £70,000 outpatient expenditure at QMR that is not attributable to patients first or follow up appointment with a practitioner, but direct access cardiology tests. The following tests are charged under direct cardiology tests: 24h BP test, 24 h tape tests, ECG, ECG report and Echo’s.
In the financial year 2012/13, the onward referrals from TMH to ICHT were just over 20%; meaning 1 in 5 LBRuT patients’ seen at TMH would be referred to ICHT for further tests or cardiology interventional procedures. Since March 2013, the provider data has demonstrated that onward referral figures to ICHT have dropped to 10%, and this value has been consistent since March 2013. However, there is no electronic database/system available to confirm these findings and the activity has been reported by the provider.
Upon review of the types of cardiology procedures being performed on LBRuT patients at ICHT, there are a number of procedures that could be performed in a district general hospital such as KHT (but not WMUH as they do not have a catheter laboratory). With the more specialist procedures it is clear that they can only be performed at a cardiac centre, however, SGH also a cardiac centre, but is not experiencing a high level of activity according to SLCSU (considering SGH is the cardiac centre for south west London, the activity is quite low).
From table 9 it is evident that the top 5 providers for cardiology, as well as cardiac services are ICHT, SGHQMR (under SGH trust), KHT, WMUH and RBH. The highest spend is with ICHT, with table x showing the actual spend for ICHT outpatient activity at over 50% more than all other providers; however, SGH has very similar numbers to ICTH in terms of outpatient activity (ICHT=1,727, SGH=1,707).
The Market Forces Factor (MFF) mentioned in the cost column (above) is an estimate of unavoidable cost difference between health care providers, based on their geographical location[li]. The MFF is used to adjust resource allocations in the NHS in proportion to these cost differences, so that patients are neither advantaged nor disadvantaged by the relative level of unavoidable costs at different providers in different parts of the country. The MFF is usually updated every year; however the MFF values for 2013/14 have been carried over to 2014/15[lii]. Therefore, costs to any services provided should not change for the next financial year.
Figure 24 Diagram to show the comparison of relative trust MFF values
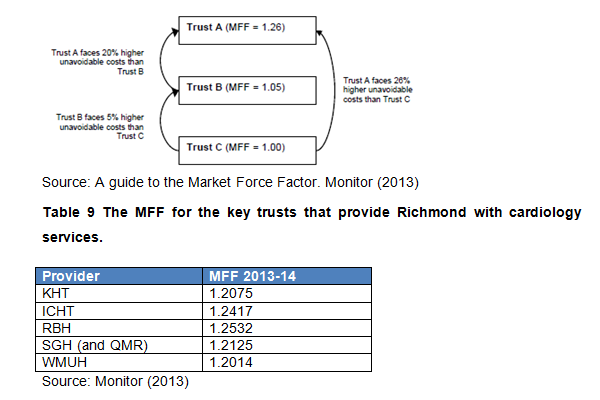
Source: Monitor (2013)
The recently issued National Tariff pricing guidance for 2014/15 indicates that national tariff prices will be slightly less in 2014/15. For more information, go to: www.monitor.gov.uk/NT
This table shows that RBH and ICHT have the highest MFF, whilst WMUH and KHT have the lowest MFF. This means that cardiology services (as well as any other services) provided by RBH and ICHT to Richmond patients will cost more than any of Richmond’s other key providers. Another point to consider is that SGH MFF is lower than SGH, yet has the facilities and expertise deliver specialist cardiology services as the cardiac centre in south London.
Onward referrals
Onward referrals to ICHT from TMH, WMUH, QMR ICHT appear to be registered as first appointments upon analysis of the patient pathways and the SUS data (table 8) which shows approximately 1,700 first appointments at ICHT, whereas no more than 5 GPs within the borough refer directly to ICHT for cardiology[liii]. Furthermore, the proportion of patients referred directly to ICHT in comparison to the overall referral numbers to cardiology services at these GP surgeries are minimal, and cannot therefore account for such a high number of first appointments at ICHT. Furthermore, ICHT is a tertiary specialist centre, which would not expect to be receiving such a high number of referrals for cardiology first appointments. It appears that patients referred on from QMR, TMH and WMUH to ICHT for further tests and treatments are booked in as first appointments at ICHT, which should not be so, as these are follow up appointments. ICHT consultants deliver the cardiology outpatient services at the above mentioned sites (QMR, TMH and WMUH), therefore, if they are referring these patients to ICHT for further investigation and/or treatment, these appointments are follow-up appointments and should be classified as such. First OP appointments cost more than follow-ups, therefore if follow-up appointments at ICHT are coded appropriately as such, that should enable some cost-savings for the CCG.
Service mapping/Gap Analysis
When conducting a review of any type of service, it is paramount to know what services currently exists, where services can be accessed, and evidently the lack of service provision. Table 11 demonstrates the key cardiology services available at key providers. However, there is variation in the provision of these services, including in terms of how many days a week these services are available, the type of diagnostics available and the profile of a 2-stop service.
Table 10 The different types of cardiology appointments available at key LBRuT providers
|
Provider |
Appointment Type |
|||||
|
Cardiology Outpatient |
1-stop/direct access |
Rapid access Chest Pain Clinic (RACPC) |
Speciality clinics, e.g. arrhythmia, HF |
Diagnostics only |
Catheter Laboratory |
|
|
ICHT (HH/CC/SMH |
X |
X |
X |
X |
X |
X |
|
KHT |
X |
X |
X |
X |
X |
X* |
|
QMR |
X |
X |
X |
X |
X |
|
|
RBH |
X |
X |
X |
X |
|
X |
|
SGH |
X |
X |
X |
X |
X |
X |
|
TMH |
X |
X |
|
X |
X |
|
|
WMUH |
X |
X |
X |
|
X |
|
* Diagnostic cardiac catheterisation only via the femoral or radial approach is performed at Kingston
Table 11 Cardiology speciality clinics available at key providers
|
Provider |
Appointment Type |
||||||
|
|
Arrhythmias |
Angina |
Atrial Fibrillation (AF) |
Coronary Artery Disease (CAD)/ (IHD) |
Hyper-tension |
Inherited Cardiac Conditions |
Heart murmur |
|
ICHT (HH/CC/SMH |
X |
|
|
|
X |
X |
|
|
KHT |
X |
|
|
|
|
|
|
|
QMR |
X |
|
|
|
X |
|
X |
|
RBH |
|
|
|
|
|
|
|
|
SGH |
X |
|
|
|
X |
X |
|
|
TMH |
X |
|
|
X |
X |
|
|
|
WMUH |
X |
|
|
|
|
|
|
Source: From provider websites and key contacts at provider sites.
The service mapping analysis shows that LBRuT patients have adequate access to arrhythmias and hypertension clinics. However, there is a lack of other specialist cardiology clinics available at key providers such as AF, and angina clinics (and these conditions can be managed within primary care).
Imaging diagnostics
For the majority of cardiology conditions, imaging is considered the main and most definitive way to obtain a diagnosis. In order to use imaging most effectively, it should be done at the relevant stages of the pathway. Also, during the referral of a patient from one provider to another, clinical bodies should ensure all results from previous diagnostic tests should be sent to the receiving clinician to avoid duplicate imaging which would have cost implications, as well as a negative impact on the patient in terms of additional time for the same procedure and unnecessary exposure to radiation.
All of the key providers for the borough, as well as LBRuT’s community cardiology service have access to the common imaging services needed to provide insight to an initial indicative diagnosis (e.g. CT, MRI, Echo), but at different prices, including the market force factor (MFF) and the fact that they are ‘unbundled’ from the outpatient appointment, and therefore charged separately.
The national tariff for Echo is £75; however, there al always additions to this price due to the type of Echo, duration of test, difference in MFFs by provider to name a few. There are no national tariffs for ECG, BP monitoring etc, so these tend to be locally negotiated prices. There is a non-mandatory price for a plain film x-ray of 25.
GPs in LBRuT currently do not follow an agreed and commonly applied suspected cardiology condition pathway or policy, therefore resulting in a wide variation in the level of referrals for different diagnostic procedures.
GPs have the freedom to send patients anywhere to conduct diagnostic tests so it is not possible to track every single service all the GPs in LBRuT refer their patients to for diagnostic procedures. It would be beneficial to have an agreed number of service providers to conduct diagnostics for NHS Richmond patients in order to keep track on where our patients go, the governance surrounding the service and the financial costs.
In the instance of laboratories that performs tests such as BNPs, the service provider is not under any obligation to provide activity data for diagnostics requested for NHS Richmond patients. This makes it more challenging to ascertain exactly how many diagnostic tests are being requested and carried out. This type of data could be easier to obtain if the CCG had an agreed number of diagnostic providers with an agreement to provide activity data periodically to the CCG for analysis.
The choice of the type of cardiac imaging diagnostic test is not always a clear choice between imaging modalities. The important determinants of which test is chosen are[liv]:
- deciding on the question(s) to be answered
- considering which of the available tests could answer the question(s)
- knowing the strengths and weakness of the available tests (which may include knowing who will do the test in some operator-dependent tests)
- The availability, cost and convenience of imaging diagnostic tests.
A well thought-out evidenced imaging strategy may well reduce the need for inappropriate imaging which will inevitably create a more targeted use of resources for patients and better outcomes[lv].
Cardiac implantable devices
In addition to the expenditure on in-patient and out-patient activity, SLCSU reported that Richmond CCG spent in the region of £838, 000 on devices associated with cardiac and cardiology related procedures. However, the data received was not 100% reflective of the costs associated with devices installed and a number of these devices will relate directly to cardiac surgery rather than cardiology.
In south west London, SGH is the only hospital in the network that can perform all three cardiac implantable device procedures that are being audited (see figure 24). However, the 2011 National Institute for Cardiovascular Outcomes Research (NICOR) audit shows that the majority of Richmond patients having these procedures took place outside of the network. The NICOR 2011 clinical audit of Heart Rhythm Devices, Pacemakers, ICD and CRT showed that St Mary’s Hospital (part of ICHT) and RBH were performing the highest numbers of procedures for LBRuT patients, with SGH usually in third or fourth place. Despite SGH being the Cardiac centre for south west London, they are recording lower device implantation numbers for the borough in comparison with ICHT and RBH. This is confirmed by the 2012/13 SLCSU reports showing that Richmond CCG spent the highest amount on devices with ICHT, followed by RBH and SGH.
Figure 25 Acute providers in south west London Cardiac and Stroke Network that are able to implant cardiac devices.
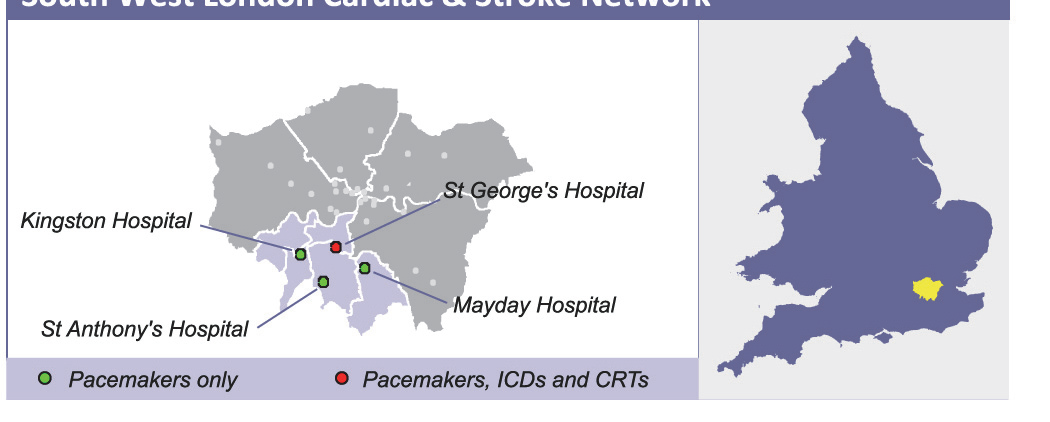
Source: National Institute for Cardiovascular Outcomes Research (NICOR) audit (2011)
The proportion of older people in a local population will strongly influence how many pacemakers need to be implanted[lvi]. Richmond has a large ageing population which is predicted to continually increase. The NHS Atlas of Variation in Healthcare (2011) shows that LBRuT had one of the highest rates of implanting pacemakers for the first time; some boroughs in London with a similar population mix also lie within the highest or second highest rates for pacemaker insertion[lvii]. Unlike pacemakers, the ICD implant rate starts to decline over the age of 75. The influence of a local elderly population of need for ICDs should still be present, but just slightly less in magnitude than for pacemakers[lviii].
Kingston CCG
Kingston CCG is currently in the process of commissioning a community cardiology service within the borough, particularly for suspected low-risk patients. This service will be delivering secondary care cardiology appointments within the community and it is intended that Richmond GPs will be able to refer patients to this service. This service will have access to a consultant cardiologist and key cardiology diagnostics available on site. This service is in the final commissioning stages and is due to being a 9-month pilot service within 2014. It will be necessary for Richmond CCG to engage with Kingston CCG and gather a better understanding about this service and what impact it could potentially have to the cardiology service provision as a number of LBRuT GPs refer patients to KHT cardiology outpatient services.
Recommendations
- Richmond CCG to consider working with Kingston CCG to create an e-proforma for suspected cardiology patients that incorporates an imaging strategy.
Kingston CCG will be setting up their community cardiology service in mid-2014, diverting a number of patients using KH outpatients to their community service. Collaborating with Kingston CCG will to develop an integrated imaging strategy with the referral proforma can reduce the need for inappropriate imaging which will foster more targeted approaches to resource allocation and improved patient outcomes. This will help reduce any inequalities that may exist with referral patterns and the preferences that exist between GPs and practices and enable the delivery of a more equitable cardiology service across the two neighbouring boroughs. This proforma should be based on recommendations from best practice guidelines and RCAS/KCAS feedback.
- Develop an integrated cardiology patient pathway
There are a number of individuals with heart disease and one or more chronic co-morbidity. These conditions need to be treated together and not in silos, as one sickness can greatly impact the progression, treatment and management of another disease. Therefore, primary care, secondary care, cardiac rehabilitation, mental health and social services need to have established links with one another to ensure that each patient is managed appropriately, simultaneously in order to avoid multiple episodes of care.
- Conduct annual audit of patients being referred to rapid access clinics this is to ensure the clinical appropriateness of the referrals that do not pass through C&B and are not reviewed by RCAS.
- Encourage and promote all routine cardiology and direct access referrals be conducted through C&B.
- However, GPs should still be able to use C&B for direct access ECGs and Holter tests without these referrals having to be approved by an RCAS assessor. The benefit of using C&B for these referrals is to capture all the cardiology activity to provide a clearer vision of the various patient pathways and referral patterns. Negotiate a lower tariff for cardiology services provided by QMR.
- Have an agreed number of service providers to conduct diagnostics for Richmond patients
Richmond CCG should consider establishing and agreement with specific diagnostic providers including the clause of providing the CCG with data on requested diagnostics for Richmond CCG population. This will facilitate the assessment of GP compliance with any agreed pathways.
- Improve CVD risk management within the community as recommended by NICE.
- Training and education for clinicians and nurses in general practice
To identify recognise cardiology conditions and associated co-morbidities that may present complications, promote CVD prevention practice and familiarise themselves with best practice recommendations for cardiology conditions.
- Improve GP access to key diagnostics needed to deliver a more comprehensive and equitable primary care cardiology service:
The GP survey showed an unequal distribution of diagnostic equipment across GP surgeries in Richmond. As a result patients are being referred to other outpatient services for diagnostic testing at an additional cost. Undertaking these tests at the GP practices could produce some cost-savings. Having these systems at the GP practice has the added benefit of eliminating delays in the overall patient pathway due to unnecessary travel to diagnostic providers. National guidelines for cardiology, including NICE, recommend that all GP practices should have the following:
- 24 hr BP monitor
- ECG machine
- All GP surgeries that currently have cardiology equipment should be encouraged to perform these tests on patients.
This would enable further cost savings and reduce delays in the patient pathway. This is particularly important since current SLA for the community cardiology service at TMH does not include conducting these tests.
- Richmond CCG should work closer with the CSU to gain better understanding of the cardiology services contracts.
- Patient information, particularly diagnostics tests and their results should be efficiently transferred from provider to provider along the patient pathway.
This will help reduce the number of repeated test, associated costs and an distress the patient may face taking repeated tests.
- The Richmond CCG should set up or nominate a cardiology implementation team to assess all recommendations and implement them accordingly.
- Richmond CCG should look into setting up a system to support GPs to conduct an annual review of patients identified as having CVD risk in excess of 20%.
This would result in a very large cohort of patients that will need following-up, and would help manage their CVD risk better for longer. However, this policy would impact greatly on resource allocation and the CCG currently does not have any system in place to support this.
Paediatric and young people’s cardiology services for Richmond patients
In 2010, around 0.8 of every 1000 babies born will suffer from some form of congenital heart disease (HD). This level of incidence leads to around 3,600 paediatric surgical procedures being performed across England every year[lix]
Congenital HD may be identified during foetal life with a very high level of diagnostic accuracy at tertiary centres[lx]. A complex network of services are therefore required for children with congenital HD that begins with prenatal screening and continues through to the transfer to adult services.
In a population of 100,000 live-born infants, the heath technology assessment ( HTA) model for new-born screening for congenital heart defects predicts that 121 infants with life-threatening congenital heart defects will be undiagnosed at screening, of whom 82 (68%) and 83 (69%) are detected by pulse oximetry and screening Echocardiography, respectively, but only 39 (32%) by clinical examination alone[lxi].
The national new-born screening policy comprises of a clinical examination at birth and 6 weeks with specific cardiac investigations for specified high-risk children. These high-risk children should be picked up antenataley or because of symptoms; however evidence shows that infants are not receiving timely management[lxii]. Early detection through newborn screening potentially can improve the outcome of congenital heart defects
Although a screening Echo is associated with the highest detection rate of congenital HD, it is the most costly strategy for identification and has a 5% false-positive rate[lxiii]. Improving antenatal detection of congenital HD increases the cost per timely postnatal diagnosis afforded by any newborn screening strategy, but does not alter the relative effects of the strategies. An improvement of timely management of screen positive infants is crucial for the health and safety of any new-born.
For pregnant women that present to their GP, factors that would increase the risk of a foetus having Congenital HD include, but are not limited to:
- Maternal Indications[lxiv]:
- Maternal congenital HD (risk 2-6%)
- Maternal metabolic disorders, especially if poor control in early gestation:
- Diabetes mellitus (risk 2-3%)
- Phenylketonuria (risk 8-10%)
- Maternal exposure to cardiac teratogens:
- Anticonvulsant, retinoic acid, lithium (risk 2%)
- viral infection (e.g. rubella) and toxoplasma
- Maternal collagen disease with anti Ro/SSA and/or anti La/SSB (Risk 2-3%)
- Maternal medication with NSAID drugs
- Drinking too much alcohol during pregnancy[lxv]
- Familial indications:
- Paternal congenital HD (risk 2-6%)
- Previous child or foetus with congenital HD or congenital heart block
- 1 affected child (risk 2-3%, though higher for some lesions, e.g. isomerism)
- 2 affected children (risk 10%)
- 3 affected children (risk 50%)
- Previous child with congenital complete heart block with maternal auto antibodies
- Child diagnoses with Down’s syndrome[lxvi]
When such risk factors have been identified, GPs should ensure that the patient details are updated with this information and refer these patients to a paediatric cardiologist.
Secondary and tertiary care paediatric services accessed by Richmond residents
St. George’s Hospital (SGH):
SGH works with Evelina Children’s Hospital paediatric cardiology service to provide close to home consultations, run screening clinics and joint clinics. Typical referrals to this service would include the accidental pick-up of a murmur, palpitations, sudden loss of consciousness, children with a documented defect on an Echo or ECG.
Cardiac Risk in the Young (CRY) is a charity that has regular cardiac testing clinics that are available free of charge to any person in the South East area and offers heart screening for 1-35 year olds. In London, the CRY screening clinic is based at the CRY Centre for Inherited Cardiovascular Conditions (ICC) and Sports Cardiology at SGH.
Queen Mary’s Hospital, Roehampton (QMR):
QMR only provides electrocardiography for paediatric cardiology patients. For comprehensive investigations and procedures the patient would be referred to ICHT. The patient could also go to SGH, but this would have to be indicated by patient choice.
West Middlesex University Hospital (WMUH)
WMUH has a paediatric consultant with special interest in cardiology that works in partnership with the tertiary paediatric team at the RBH. As a result cardiology services have now been working in a more integrated way with the hospital paediatrics service and are able to deliver more services in terms of Echo, ECG and ECG holter monitoring on site, before referral to a tertiary centre (if necessary). The provider hosts a monthly outreach clinic delivered by an RBH consultant paediatrician. WHUM also has a physiologist from RBH to develop complex Echo skills needed to perform the diagnostic test on children. The hospital runs a cardiology obstetric MDT which includes input from cardiology, obstetrics & gynaecology, paediatrics and obstetric anaesthesia to improve cardiovascular outcomes for pregnant women. Specialist paediatric cardiology or grown up congenital heart disease (GUCH) patients are referred to RBH.
In 2012/13, South London Commissioning Support Unit (SLCSU) reported that RCCG’s highest spend with its key providers for paediatric cardiology was with WMUH at £7,557 (in comparison with ICHT at £2,056 and SGH at £930). It is believed this is as a result of increased outpatient activity and diagnostics due to the addition of a paediatric cardiologist at WMUH.
Royal Brompton Hospital (RBH):
RBH specialises in cardiothoracic services for all stages of life, and therefore has a number of diagnostic equipment, as well as specialist physicians that can diagnose, treat and manage patients from foetus stage till adult life. The hospital has an on-site foetal cardiology service facilitating the care for babies while still in the womb.
Imperial College Healthcare Trust (ICHT):
St Mary’s and Queen Charlotte’s & Chelsea hospitals both offer an outpatient paediatric cardiology service, provided by joint clinics with the RBH paediatric cardiology department; this service includes:
- Outpatient screening and review of children or new-borns with suspected congenital or acquired heart disease
- investigation of cardiac murmurs, dysrhythmias, and chest pain
- 24-hour ambulatory blood pressure monitoring(ABPM)
- 24-hour ECG heart monitoring for all age groups
- Inherited Cardiac Conditions (ICC) service
Great Ormond Street Hospital (GOSH):
It is the largest centre for child heart surgery in the UK and one of the largest centres for heart transplantation in the world. Children are treated from birth until adolescence when they are transferred to the Grown Up Congenital Heart Unit (GUCH). The team provides a tertiary referral service both nationally and internationally and have close clinical links with University College London (UCL) and the Cardiology in the Young service at the Heart Hospital, UCL.
GOSH offers a full range of National Commissioning Group (NCG) specialist cardiac services including ECMO, bridge to transplant, , tracheal services and pulmonary hypertension, catheter laboratory for cardiac and pulmonary disease, electrophysiology (EP) service and offers a full range of diagnostic and therapeutic interventions for primary arrhythmias in children.
The Foetal Cardiac Service provides services for the diagnosis, counselling and management of prenatal cardiac disease and is an interface between the paediatric cardiothoracic services and maternal health units throughout London and across the UK; this service is based across two sites: at GOSH and with an integrated foetal cardiology-foetal medicine service at UCLH.
Evelina Children’s Hospital (Part of St Thomas’s and Guys NHS Trust):
The Department of Congenital Heart Disease at the Evelina Children’s Hospital diagnoses and treats patients of all age groups with heart problems from the foetus to adult life.
Besides the standard Echocardiography, transoesophageal Echocardiography can be needed and this investigation may be performed in the hospital day case ward.
Costs and activity
The South London Commissioning Support Unit (SLCSU) reported that Richmond Clinical Commissioning Group (RCCG) spent £10,543 with its key providers for only paediatric cardiology in 2012/13. However, Richmond Public Health intelligence (PHI) have utilised the activity data from CSU SUS, the agreed tariff for first appointments and follow-up appointments and the MFF factor to calculate the estimated costs for reported Richmond activity at all London providers for paediatric cardiac surgery and paediatric cardiology in 2012/13. The estimated total costs of paediatric cardiac surgery and paediatric cardiology for 2012/13 came to the amount of £112,552 in 2012/13.
Table 13 (below) shows Richmond activity for paediatric cardiac surgery and paediatric cardiology activity in 2012/13. It is important to note that the activity and costs below include appointments for patients that specifically need cardiac surgery and their associated follow up. The cost value reported by SUS is an estimated amount that relates directly to the activity that the acute providers report.
Table 12 Activity and associated costs for all treatment functions for paediatric cardiac surgery and paediatric cardiology 2012/13.
|
First Attendance |
Follow up |
Procedure |
||||
|
Provider |
Attendances |
Cost Incl. MFF |
Attendances |
Cost Inc MFF |
Attendances |
Cost Inc MFF |
|
RBH |
89 |
£ 23,710 |
191 |
£34,946 |
||
|
GOSH |
23 |
£5,941 |
135 |
£23,466 |
||
|
GSTT |
6 |
£1,686 |
17 |
£3,313 |
11 |
£4,102 |
|
C&W |
16 |
£4,555 |
8 |
£1,511 |
1 |
£180 |
|
WMUH |
21 |
£5,551 |
3 |
£526 |
||
|
ICHT |
5 |
£1,366 |
1 |
£181 |
||
|
RMH |
– |
– |
4 |
£709 |
||
|
SGH |
2 |
£487 |
1 |
£146 |
||
|
BH |
– |
– |
1 |
£177 |
||
|
KHT |
– |
– |
|
|
|
|
|
Total |
162 |
£43,294 |
361 |
£64,976 |
12 |
£4,282 |
Source: Richmond Public Health Analysis using SUS data, 2012/3
Form this table it is evident that Richmond’s top five key providers for paediatric cardiology and cardiac surgery are RBH, GOSH, WMUH, C&W, GSTT. This is expected as RBH and GOSH is well-established tertiary specialist centres for paediatric cardiology, whilst WMUH are able to conduct diagnostic tests and outpatient paediatric appointments.
References
[1] Refractory angina = patients who have stable angina in whom revascularisation is either unfeasible or where risks are unacceptable (est 0.2% population)
[2] Palliative PCI = revascularisation by PCI (percutaneous coronary intervention with balloons or stents) method for symptom control, rather than for prognostic (life-prolonging) purposes
[i] National Heart, lung and blood Institute (NIH) (2011) Whart are the signs and symptoms of heart disease? NIH
[ii] National Institute for Health and Clinical Excellence (NICE) (2011) Hypertension: clinical management of primary hypertension in adults. NICE.
[iii] British Heart Foundation (BHF)
[iv] Map of Medicine (MoM) (2010) Acute coronary syndrome- suspected, MoM
[v] Scottish Intercollegiate Guidelines Network (SIGN) (2012) Acute Coronary Syndromes. SIGN
[vi] Scottish Intercollegiate Guidelines Network (SIGN) (2012) Acute Coronary Syndromes. SIGN
[vii] National Institute of Health and Clinical Excellence (NICE (2010) Chest pain of recent offset. NICE
[viii] Scottish Intercollegiate Guidelines Network (SIGN) (2012) Acute Coronary Syndromes. SIGN
[ix] National Institute of Health and Clinical Excellence (NICE (2010) Chest pain of recent offset. NICE
[x] British Heart Foundation (BHF) (2013) Angina. BHF
[xi] National Institute of Health and Clinical Excellence (NICE (2010) Chest pain of recent offset. NICE
[xii] Faculty of Public Health and the National Heart Forum (2005) Easing the pressure: tackling hypertension.
[xiii] Joint Health Surveys Unit. (2004) Risk factors for cardiovascular disease. Volume 2. Health Survey for England .
[xiv] Faculty of Public Health and the National Heart Forum (2005) Easing the pressure: tackling hypertension.
[xv] NICE (2011) Hypertension NICE
[xvi] National Institute for Health and Clinical Excellence (NICE) (2010) Prevention of cardiovascular disease. NICE
[xvii] The Health Foundation ( Healthcare delivery models for prevention of cardiovascular disease (CVD)
[xviii] National Institute for Health and Clinical Excellence (NICE) (2010) Lipid modification. NICE
[xix] Hippisley-Cox, J et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:a332
[xx] National Institute for Health and Clinical Excellence (NICE) (2014) Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease – Draft for consultation. NICE
[xxi] Greater Manchester
[xxii] Skipsey, DA et al. (2012) Evaluation of a direct access cardiac arrhythmia monitoring service. Vol. 19, No. 1, pp. 70–75.
[xxiii] Skipsey, DA et al. (2012) Evaluation of a direct access cardiac arrhythmia monitoring service. Vol. 19, No. 1, pp. 70–75.
[xxiv] Skipsey, DA et al. (2012) Evaluation of a direct access cardiac arrhythmia monitoring service. Vol. 19, No. 1, pp. 70–75
[xxv] British Heart Foundation (BHF) (2013) Hearth Rhythms.
[xxvi] Resuscitation Council UK (2010) Resuscitation guidelines 2010. Resus UK
[xxvii] Scottish Intercollege Guidelines Network (SIGN) (2012) Acute Coronary Syndromes. SIGN
[xxviii] Scottish Intercollege Guidelines Network (SIGN) (2012) Acute Coronary Syndromes. SIGN
[xxix] National Institute for Health and Clinical Excellence (NICE) (2006) Implantable cardioverter defribrillators for arrhythmias. Technology Appraisal 95. NICE
[xxx] Scottish Intercollege Guidelines Network (SIGN) (2012) Acute Coronary Syndromes. SIGN
[xxxi] Scottish Intercollege Guidelines Network (SIGN) (2012) Acute Coronary Syndromes. SIGN
[xxxii] British Heart Foundation (BHF) (2008)Heart Murmurs. BHF
[xxxiii] Map of Medicine (MoM) (2012) Valvular Heart Disease. MoM
[xxxiv] Richmond Annul Public Health Report 2013
[xxxv] National Service Framework (NSF) (2004) Winning the War on Heart Disease. NSF
[xxxvi] London Borough of Richmond upon Thames (LBRuT) 2012. Joint Strategic Needs Assessment – Older People Needs Assessment Summary, LBRuT.
[xxxvii] London Borough of Richmond upon Thames (LBRuT) 2012. Joint Strategic Needs Assessment – Older People Needs Assessment Summary, LBRuT.
[xxxviii] London Borough of Richmond upon Thames (LBRuT) 2012. Joint Strategic Needs Assessment – Older People Needs Assessment Summary, LBRuT.
[xxxix] London Borough of Richmond Upon Thames (LBRuT) 2012. Joint Strategic Needs Assessment – Older People Needs Assessment Summary, LBRuT.
[xl] London Borough of Richmond Upon Thames (LBRuT) 2012. Joint Strategic Needs Assessment – Older People Needs Assessment Summary, LBRuT
[xli] LBRuT GP questionnaire (2013)
[xlii] National Service Framework (NSF (2000) Coronary Heart Disease. NSF.
[xliii] National Institute of Health and Clinical Excellence (NICE) (2010) Lipid modification
[xliv] European Society of Cardiology (ESC) (2013) Task Force on the management of stable coronary artery disease. ESC.
[xlv] European Society of Cardiology (ESC) (2013) Task Force on the management of stable coronary artery disease. ESC.
[xlvi] Wright CA Osborn DP, Nazareth I, King MB. Prevention of coronary heart disease in people with severe mental llnesses: a qualitative study of patient and professionals’ preferences for care. BMC Psychiatry 2006; 6: 16
[xlvii] Scottish Intercollegiate Guidelines Network (SIGN) (2012) Heart Disease SIGN
[xlviii] London Health Programmes (LHP) (2010) Cardiovascular Project. Proposed model of care. LHP
[xlix] National Institute for Health and Clinical Excellence (NICE) (2006) Atrial Fibrillation. NICE
[l] South London Commissioning Support Unit (SL CSU), 2012-13.
[li] Monitor (2013). A guide to the Market Forces Factor. Monitor
[lii] Monitor (2013). A guide to the Market Forces Factor. Monitor
[liii] Richmond GP survey (2013)
[liv] Department of Health (DH) National Imaging Board (2010) Cardiac Imaging. DH
[lv] Department of Health (DH) National Imaging Board (2010) Cardiac Imaging. DH
[lvi] National Institute for Cardiovascular Outcomes Research (NICOR) (2011) Clinical Audit of Heart Rhythm Devices.
[lvii] Right Care (2011) The NHS Atlas of Variation in Healthcare. Rightcare.
[lviii] National Institute for Cardiovascular Outcomes Research (NICOR) (2011) Clinical Audit of Heart Rhythm Devices.
[lix] National Specialised Commissioning Group (NSCG) (2010) Paediatric Congenital Cardiac Services in England. NSCG
[lx] British Congenital Cardiology Association (BCCA) (2012) Fetal Cardiology Standards. BCCA
[lxi] Health Technology Assessment (HTA) (2005) Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.Vol.9 No.44. HTA
[lxii] Health Technology Assessment (HTA) (2005) Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.Vol.9 No.44. HTA
[lxiii] Health Technology Assessment (HTA) (2005) Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.Vol.9 No.44. HTA
[lxiv] British Congenital Cardiology Association (BCCA) (2012) Fetal Cardiology Standards. BCCA
[lxv] NHS Wales (2014) Congenital Heart Disease. NHS Wales
[lxvi] NHS Wales (2014) Congenital Heart Disease. NHS Wales
Document Information
Published: March 2014
For review: March 2017
Topic lead: Usman Khan, Public Health Principal
Appendices
Appendix 1. Membership of Cardiology Pathway Steering and Working Group
Steering Group
|
Name |
Title |
Organisation |
|
Dr. Nicola Bignell |
Richmond CCG Governing Body member and GP |
NHS Richmond CCG |
|
Dr. Patrick Gibson |
GP with Special Interest |
NHS Richmond CCG |
|
Dr. Alexander Norman |
Clinical lead for review and GP with Special Interest |
NHS Richmond CCG |
|
Anna Raleigh |
Consultant in Public Health |
London Borough of Richmond upon Thames (LBRuT) |
|
Dr. Usman Khan |
Public Health Principal |
LBRuT |
|
Oliver McKinley |
Clinical Commissioning Manager |
LBRuT |
|
Angela Aboagye |
Public Health Lead |
LBRuT |
|
Chirag Patel |
Senior Practice Pharmacist |
NHS Richmond CCG |
|
Carol McLoughlin |
Senior Commissioning Manager |
NHS South London Commissioning Support Unit (SLCSU) |
|
Peter Yuen |
Public Health Analyst |
LBRuT |
|
Julie Read |
Respiratory & Cardiac Rehabilitation Clinical Services Manager |
Hounslow & Richmond Community Healthcare NHS Trust (HRCH) |
Working Group
|
Name |
Title |
Organisation |
|
Dr. Alexander Norman |
Clinical lead for review and GP with Special Interest |
NHS Richmond CCG |
|
Dr. Usman Khan |
Public Health Principal |
LBRuT |
|
Oliver McKinley |
Clinical Commissioning Manager |
LBRuT |
|
Angela Aboagye |
Public Health Lead |
LBRuT |
|
Chirag Patel |
Senior Practice Pharmacist |
NHS Richmond CCG |
|
Peter Yuen |
Public Health Analyst |
LBRuT |
|
Leona Patel |
Public Health Lead |
LBRuT |
Appendix 2. GP Cardiology Services and Provision in Richmond Questionnaires (LPIS) 2013.
|
1. What serviceable cardiology equipment do you hold within your practice (e.g. 24hr BP, ECG/24hr ECG)? Please specify brand and model |
|
2. Where does your practice refer cardiology patients to and why? Please specify site/provider |
|
3. Do you use a ‘1-stop’ (rapid access) service or do you refer for diagnostics and then work up the patient yourself? |
|
4. Would you be interested in an incentive scheme for AF screening e.g. in Health Checks; what other service/activity would you consider delivering within such a scheme? |
|
5. What does your practice do with post-cardiac event patients discharged from secondary care? |
|
6. What cardiac rehab services are you aware of within your area and do you refer patients to them? |
|
7. What could secondary care do to help you with your on-going care of cardiology patients within your practice? |
|
8. Any other comments relating to cardiology services and provision? |
Appendix 3. Map of Medicine care pathway for suspected acute coronary syndrome (ACS)
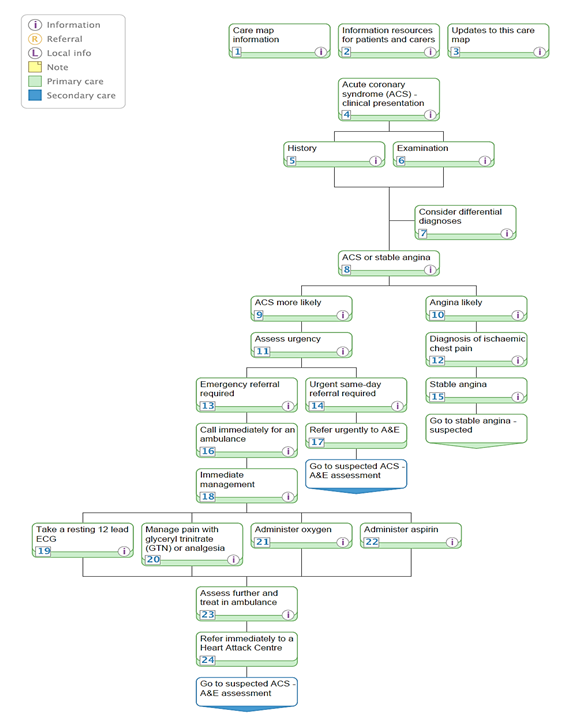
Appendix 3. Map of Medicine care pathway for stable angina at presentation
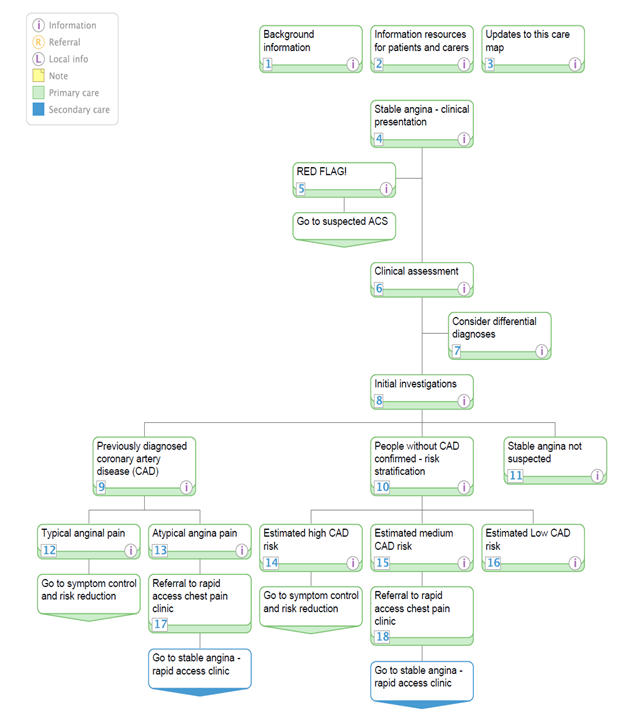
Appendix 4. Map of Medicine care pathway map for cardiovascular disease (CVD) risk assessment and primary prevention
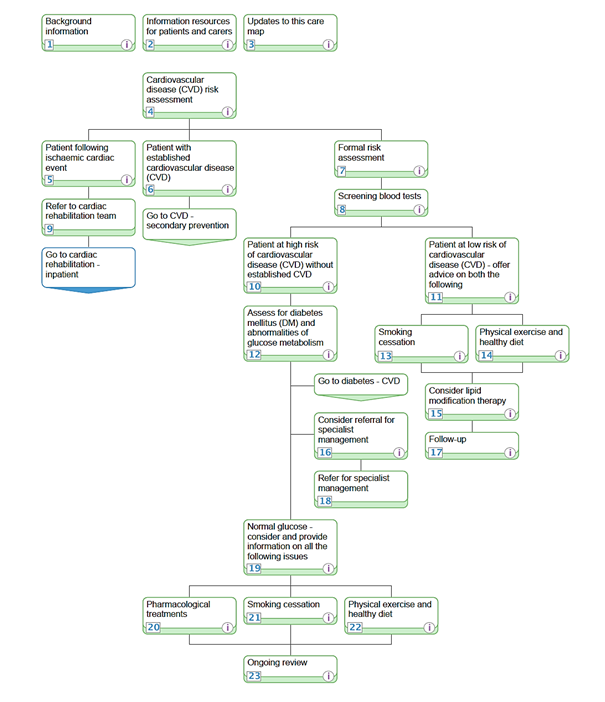
Appendix 5. Map of Medicine care pathway for suspected Hypertension
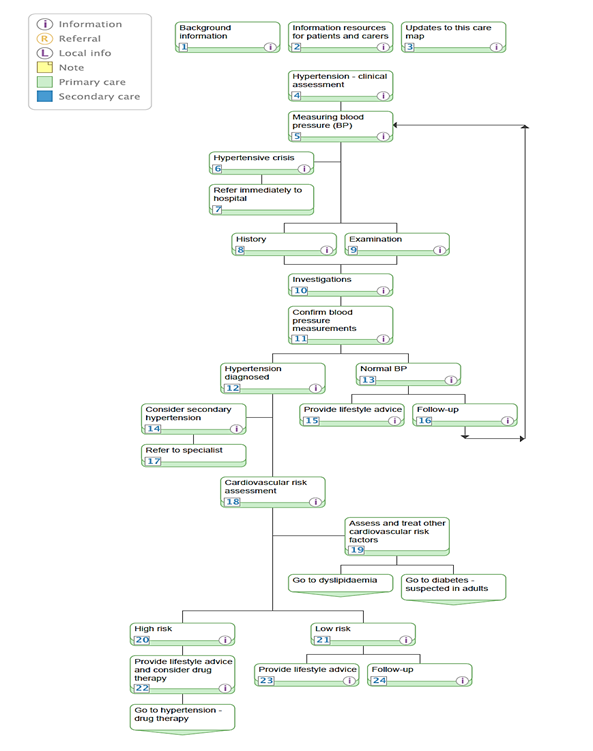
Appendix 6. Patient referral profile for Richmond community cardiology services at Teddington Memorial Hospital (TMH) by Imperial College Healthcare Trust (ICHT)
|
Guidance on referring – Patient Profile
|
Tests done prior or during appointment by Imperial |
||
|
Chest pain
|
Chest pain on exertions or shortness of breath on exertion Refer to general cardiology
|
Patients who experience chest pain at rest will need to go to A&E |
ECG Exercise Test Echo- (if clinically indicated) |
|
Palpitation
|
Palpitations without loss of conscience or falls – Refer for GP access direct 24hr tape which will be reported and future plan advised in report
|
Palpitations with loss of conscience /falls/ symptomatic Refer to General Cardiology clinic |
ECG Echo 24hr tape/ cardio-memo
|
|
Arrhythmia
|
History/probable history of arrhythmia: Suggest GP access direct 24hr ECG monitoring or cardio memo in the first instance. Refer for GP access 24hr ECG and results will be reported. |
Documented Arrhythmia/ Non- documented arrhythmia but clinical history strongly suggests arrhythmia Refer to General Cardiology with documented evidence of arrhythmia
|
ECG Echo 24hr tape/ cardio-memo |
|
Heart Failure
|
Refer to General Cardiology clinic
|
|
ECG Echo
|
|
Hypertension
|
Newly diagnosed prior to commencement of medication ?White Coat syndrome Refer for GP access 24hr BP and results will be reported. |
Refer to General Cardiology clinic for difficult to manage patients. |
ECG Echo- (if clinically indicated) 24hr Blood pressure |
